WORLD HEART REPORT 2024
CLEARING THE AIR TO ADDRESS POLLUTION’S CARDIOVASCULAR HEALTH CRISIS
1. EXECUTIVE SUMMARY

EVERYONE IS EXPOSED TO AIR POLLUTION THROUGHOUT THEIR LIVES, NO MATTER WHERE THEY LIVE IN THE WORLD. ITS IMPACTS ARE FAR-REACHING – FROM CAUSING AND EXACERBATING ILL HEALTH, TO LOSS OF LIFE.
In 2019, almost 7 million deaths were attributed to air pollution.
READ MORE
Together, ambient and household air pollution contribute to more deaths than all wars, malaria, tuberculosis, HIV, and other infectious diseases combined.
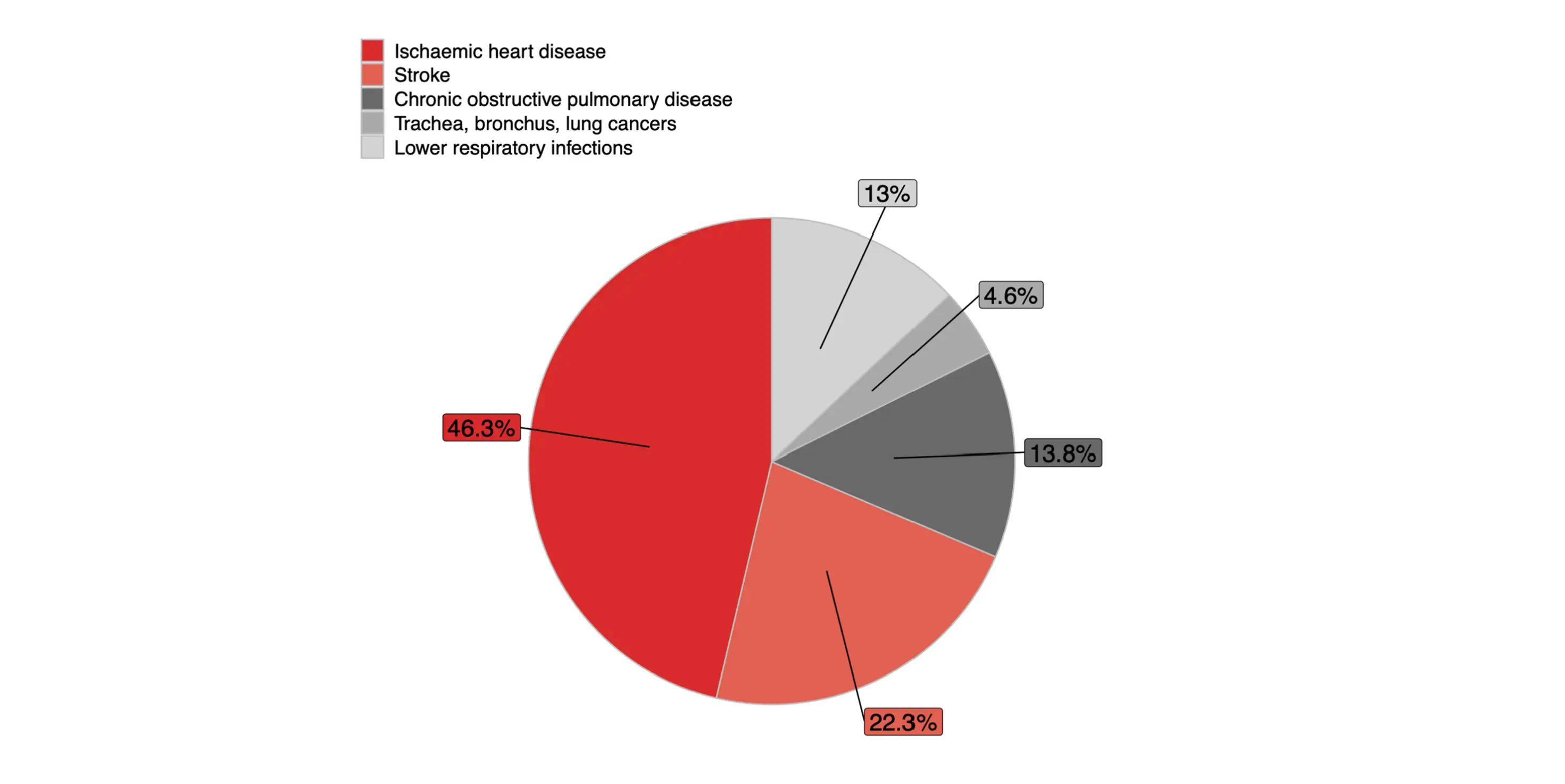
Exposure to air pollution is linked to the exacerbation of all major cardiovascular diseases (CVDs). Almost 70% of the 4.2 million deaths in 2019 attributed to ambient air pollution were caused by cardiovascular conditions, notably ischaemic heart disease (IHD) (1.9 million deaths) and stroke (900,000 deaths).
Out of the 3.2 million deaths attributed to household air pollution in 2019 – 1 million deaths were from IHD and 700,000 from stroke. Globally, 22% of deaths from IHD and 15% from stroke were attributable to air pollution in 2019.
The ubiquity of air pollution exposure and its effects on cardiovascular health represents a staggering challenge for global health. Within the global picture of air pollution and CVDs is a story of significant regional and country differences. As with many other areas of health, lower-income countries bear a disproportionate burden.
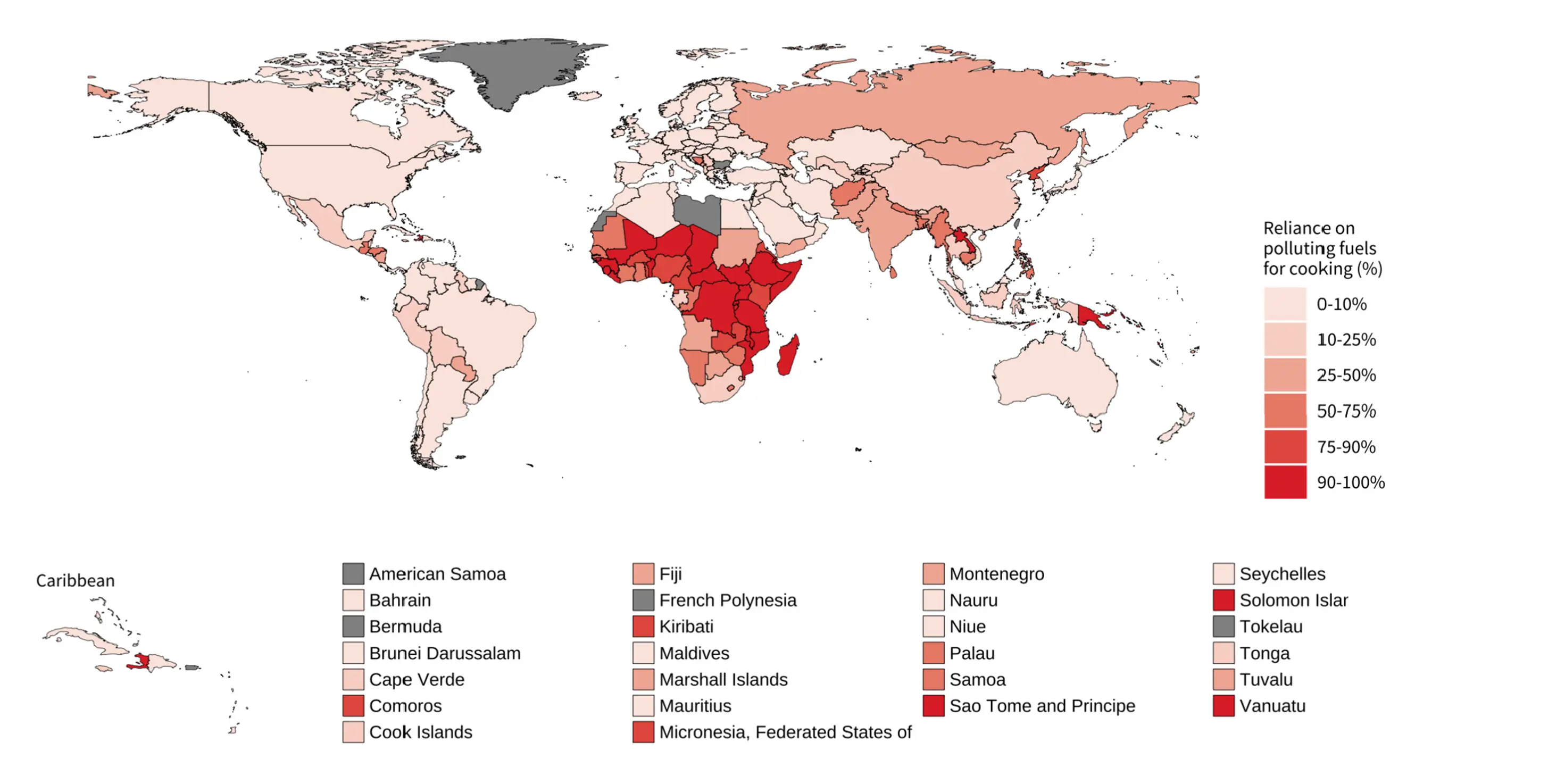
World Health Organization (WHO) estimates that over 2 billion people worldwide still rely on polluting fuels, such as wood, coal, crop waste, or charcoal paired with inefficient stoves for cooking.
Despite the awareness of air pollution harms, particulate matter (PM) 2.5 concentration levels—the key pollutant for human health—declined globally by just 1% annually between 2010 and 2019. Global levels remained alarmingly high at 31.7 µg/m in 2019, far above the 2021 WHO recommended air quality guidance level of 5 µg/m3.
Read the full Executive Summary here.
AN URGENT NEED FOR COMPREHENSIVE STRATEGIES
Many air pollution interventions will also help tackle the climate crisis, and the health benefits of reducing air pollution far outweigh the economic requirements to achieve them.
OVER 2 BILLION PEOPLE WORLDWIDE STILL RELY ON POLLUTING FUELS
ALMOST 7 MILLION DEATHS FROM AIR POLLUTION
THIS REPORT PROVIDES THE FOLLOWING KEY RECOMMENDATIONS:
- All countries must adopt the new WHO global guidelines on air quality.
- WHF supports the implementation of a global fossil fuel non-proliferation treaty.
- Countries and technical bodies, particularly in low- and middle-income countries (LMICs), should urgently improve air pollution monitoring and modelling where there are gaps.
- Countries must ensure increase funding for multidisciplinary air pollution research and technological innovations to improve air quality and develop strategies to implement interventions to reduce air pollution.
- Additional studies need to be conducted into the cardiovascular effects of air pollution and how CVDs are linked to ambient and household air pollution, in addition to the role of the cardiovascular system in the disease of other organs.

2. INTRODUCTION

Air pollution—which has been shown to have damaging effects on most organs of the body—is the sixth biggest risk factor for mortality globally, the seventh for disability-adjusted life years (DALYs)*, and the number one environmental risk factor for ill health and death [1].
The impacts of air pollution on cardiovascular health are profound, with exposure linked to the exacerbation of all major CVDs, including IHD and stroke.
* One DALY represents the loss of the equivalent of one year of full health. DALYs for a disease or health condition are the sum of the years of life lost (YLLs) to due to premature mortality (YLLs) and the years lived with a disability (YLDs) due to prevalent cases of the disease or health condition in a population.

Caption example
READ MORE
The World Bank estimates that the global cost of health damages associated with exposure to air pollution is US$8.1 trillion, equivalent to 6.1% of the global GDP, with 1.2 billion annual workdays lost [2]. Predictions indicate that global air pollution-related healthcare costs will surge from US$21 billion in 2015 to US$176 billion in 2060 [3].
Read the full Introduction here.
This second World Heart Report (WHR) is aimed at equipping policymakers and advocates around the world with a consolidated analysis of the interplay between air pollution and CVDs, with the goal of identifying areas for concrete action that will mitigate air pollution’s harms not only on cardiovascular health but also overall health.
3. GLOBAL LEVELS/TRENDS OF AMBIENT AIR POLLUTION

THE LARGEST PM2.5 DECLINE WAS RECORDED IN EUROPE (2.1% AVERAGE ANNUAL CHANGE).
PM2.5 LEVELS INCREASED ANNUALLY BY 0.3% IN AFRICA.
THE LARGEST RELATIVE DECLINES WERE OBSERVED IN MOST EUROPEAN COUNTRIES.
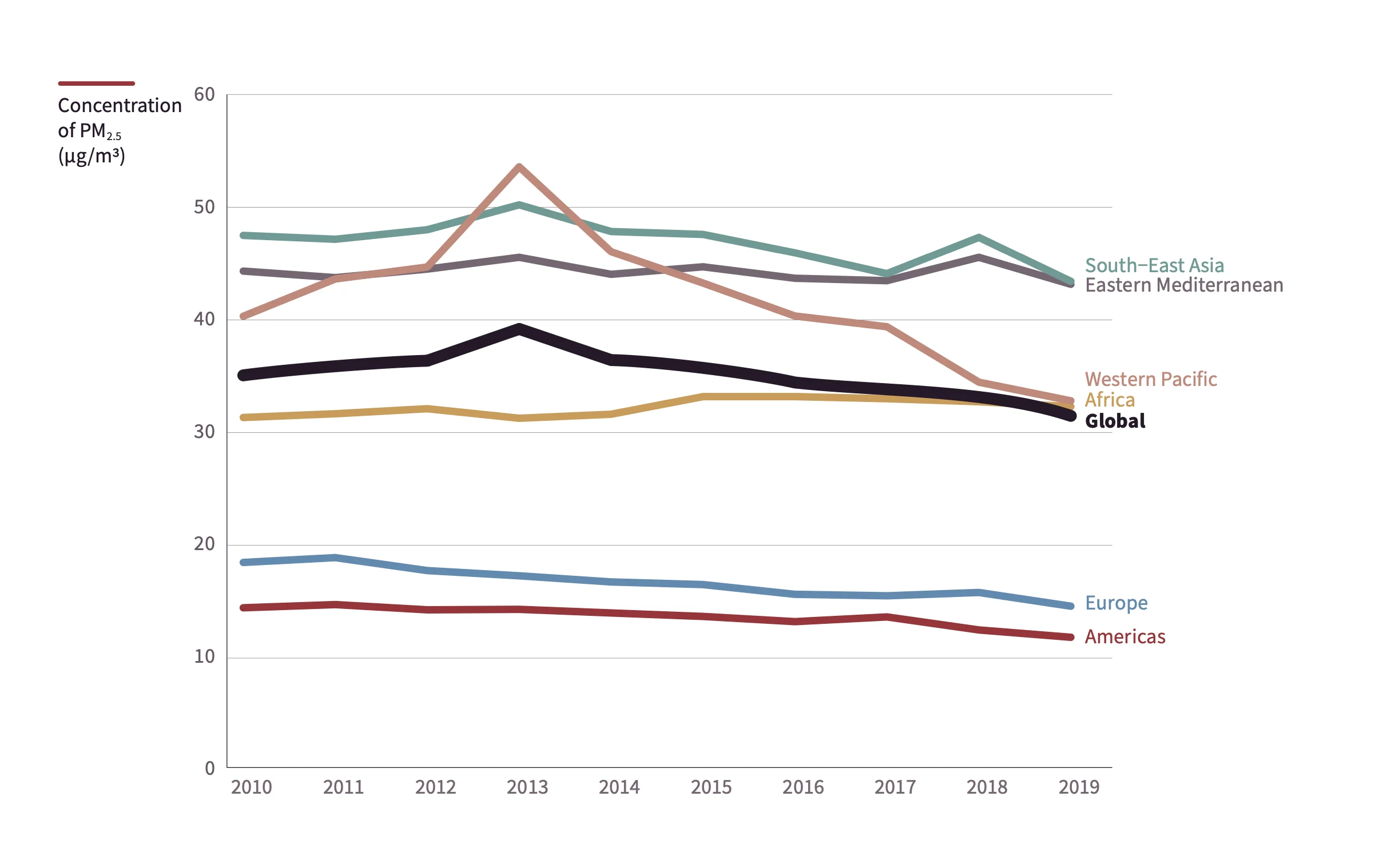
FIGURE 2 - Trends in mean annual PM2.5 concentrations by WHO regions, 2010-2019. Source: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/concentrations-of-fine-particulate-matter-(pm2-5)
THE LARGEST RELATIVE INCREASES WERE RECORDED IN ANGOLA (12.2%), CABO VERDE (10.3%), LIBERIA (8.9%), SIERRA LEONE (8.5%), AND PALAU (8.2%).
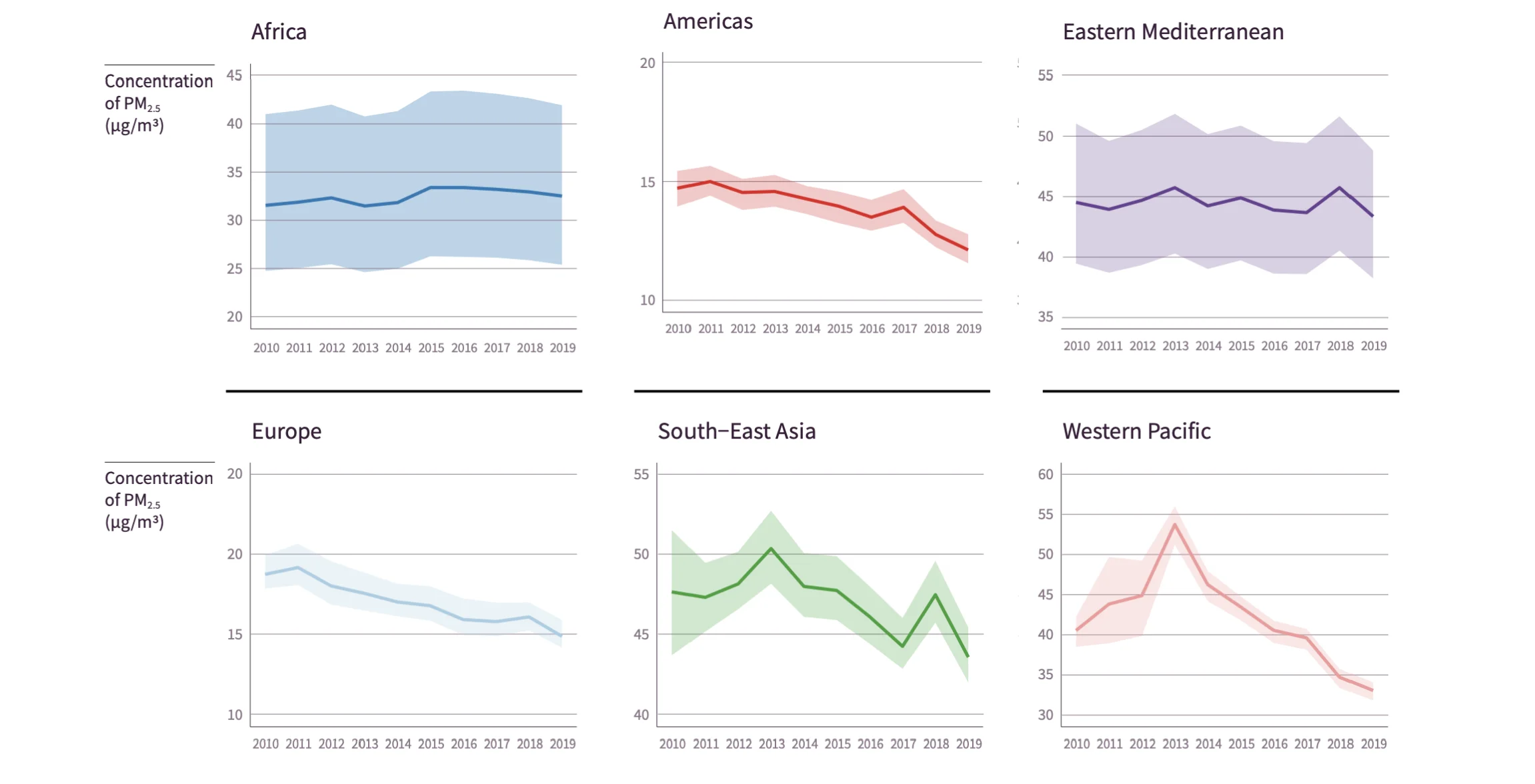
FIGURE 2.1 - Trends in mean annual PM2.5 concentrations by WHO regions, 2010-2019. Source: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/concentrations-of-fine-particulate-matter-(pm2-5)
All countries in the Europe and South-East Asia regions experienced a decline in PM2.5 levels between 2010 and 2019, while 60% of the countries in Africa observed an increase. In the Eastern Mediterranean, Americas, and Western Pacific regions, 36%, 43%, and 45% of countries, respectively, recorded an increase in the level of PM2.5 concentration.
In 2019—the most recent WHO data on record—no country in the world had PM2.5 concentrations below this threshold.
READ MORE
The highest levels of annual average PM2.5 concentrations were recorded in the Global South, with the highest levels in Kuwait (64.1 µg/m3; Confidence Interval [CI] 55.7-72.5), Egypt (63.2µg/m3; CI 40.4-92.3), and Afghanistan (62.5 µg/m3; CI 45.0-86.5). Countries with the lowest levels of PM 2.5 concentration were the Bahamas (5.2µg/m3; CI 3.8-7.1), Finland (5.5 µg/m3; CI 5.2-5.8), Iceland (5.8 µg/m3; CI5.1-6.5), and Sweden (6.0 µg/m3; CI 5.7-6.2).
Read the full findings on Global levels/trends of ambient air pollution here.
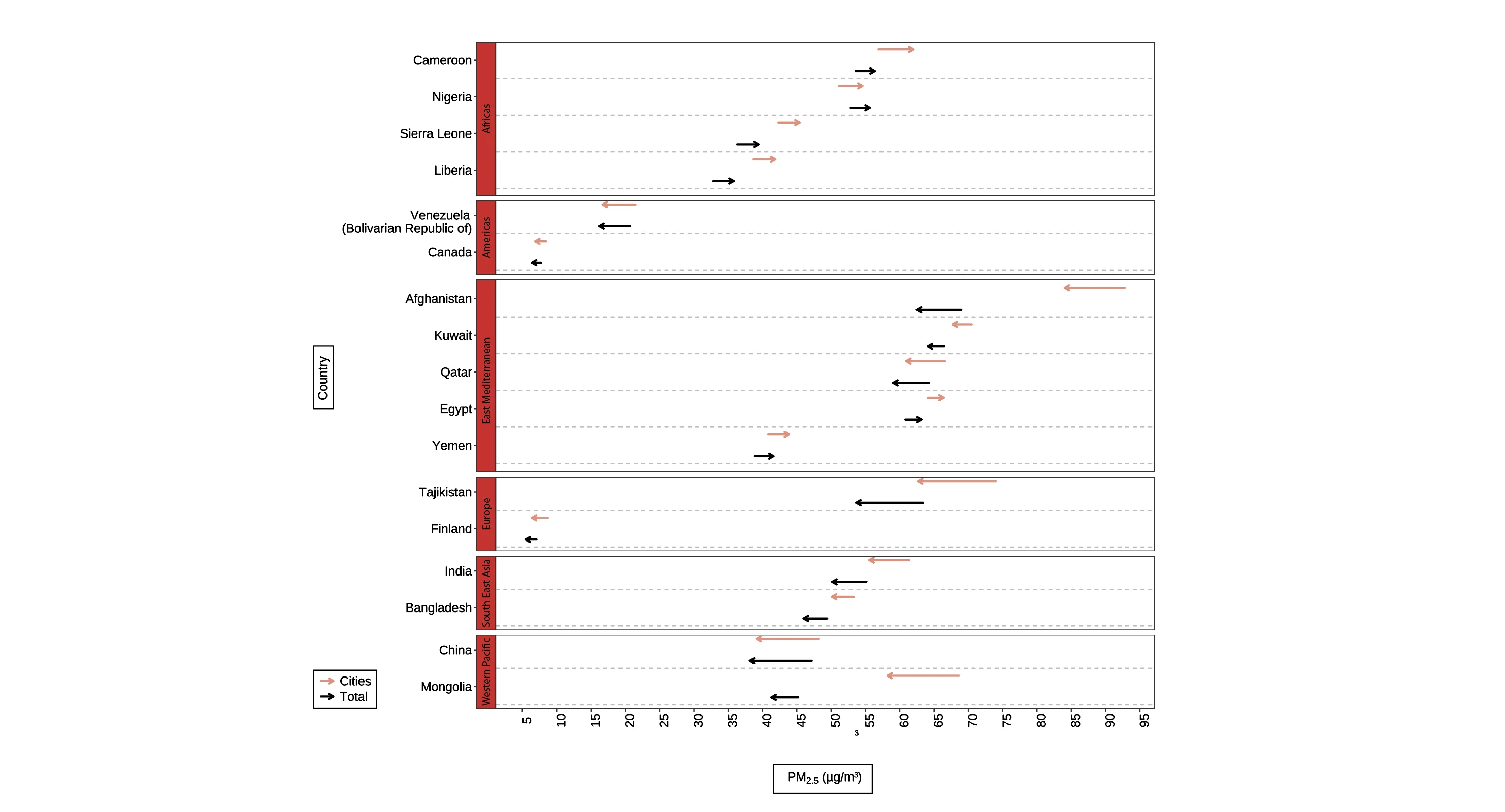
FIGURE 3 - Changes in PM2.5 concentrations between 2010 and 2019 (selected countries; overall and city-level). Source: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/concentrations-of-fine-particulate-matter-(pm2-5)

NO COUNTRIES IN THE AFRICA, EASTERN MEDITERRANEAN, OR SOUTH-EAST ASIA REGIONS RECORDED AN AVERAGE ANNUAL PM2.5 CONCENTRATION BELOW 10 µG/m3.
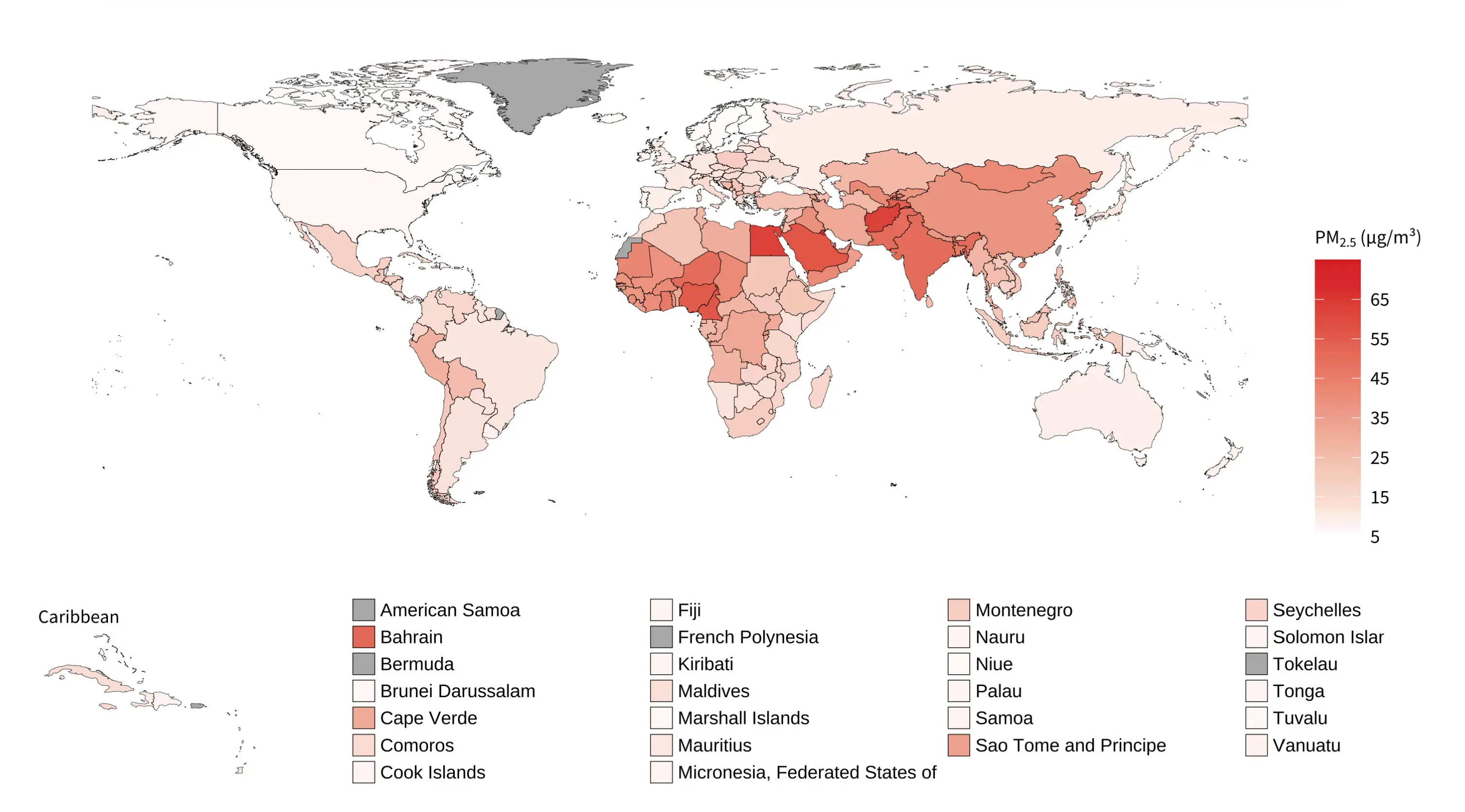
FIGURE 4 - Mean annual PM2.5, 2019. Source: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/concentrations-of-fine-particulate-matter-(pm2-5)
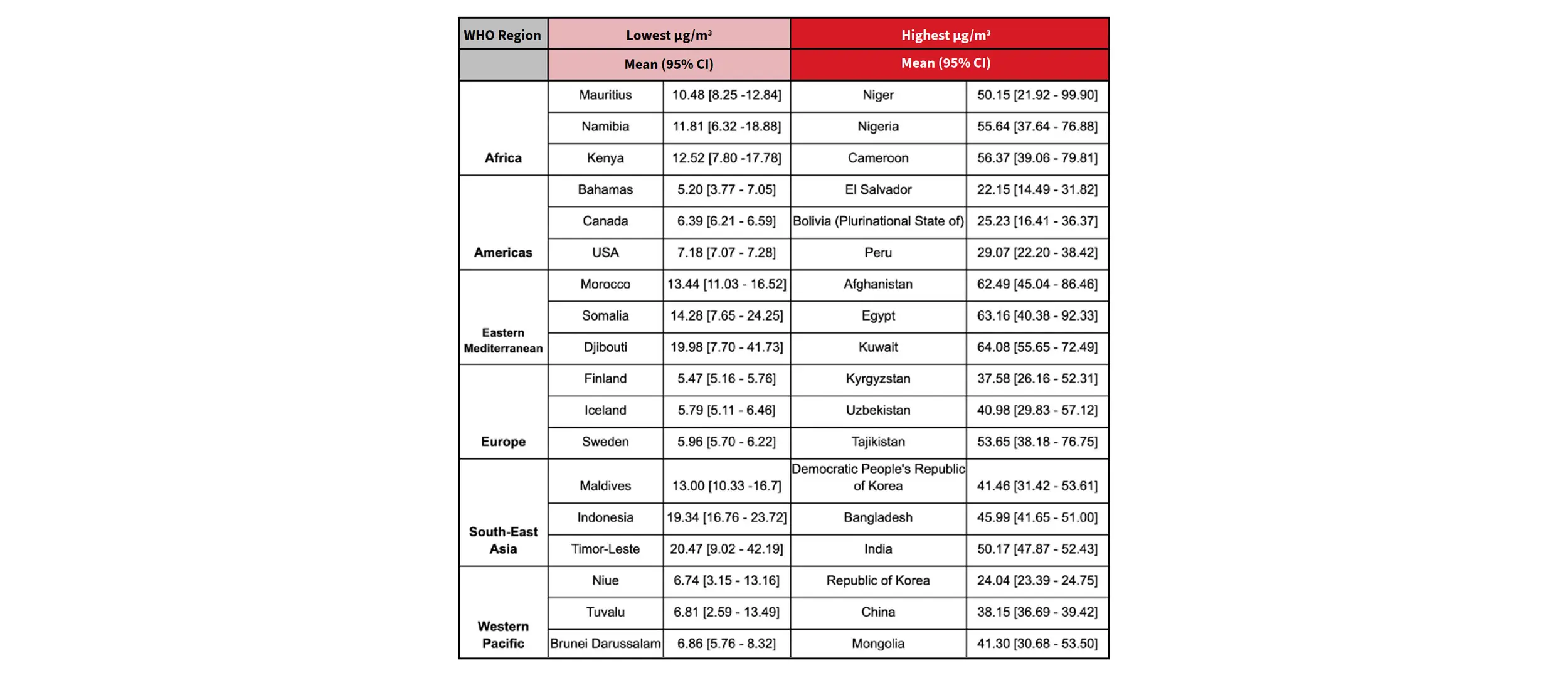
TABLE 1 - PM2.5 levels: Lowest and highest 3 countries by WHO regions (2019). Source: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/concentrations-of-fine-particulate-matter-(pm2-5)
4. AMBIENT AIR POLLUTION AND HEALTH

Ambient air pollution is currently the sixth biggest risk factor for mortality globally, the seventh for DALYs, and the number one environmental risk factor.
READ MORE
In 2019, ambient air pollution caused 4.2 million deaths and over 100.4 million DALYs. The number of deaths was almost 140,000 more than the number recorded in 2010, a rise mostly driven by the South-East Asia (152,000 more deaths), Western Pacific (64,000 more deaths) and Eastern Mediterranean (47,000 more deaths) regions. Europe recorded over 135,000 fewer deaths in 2019 compared to 2010. Research over the last decade has found associations between air pollutants and conditions of most organs of the body. [11]
Read the full findings around the Ambient air pollution and health here.
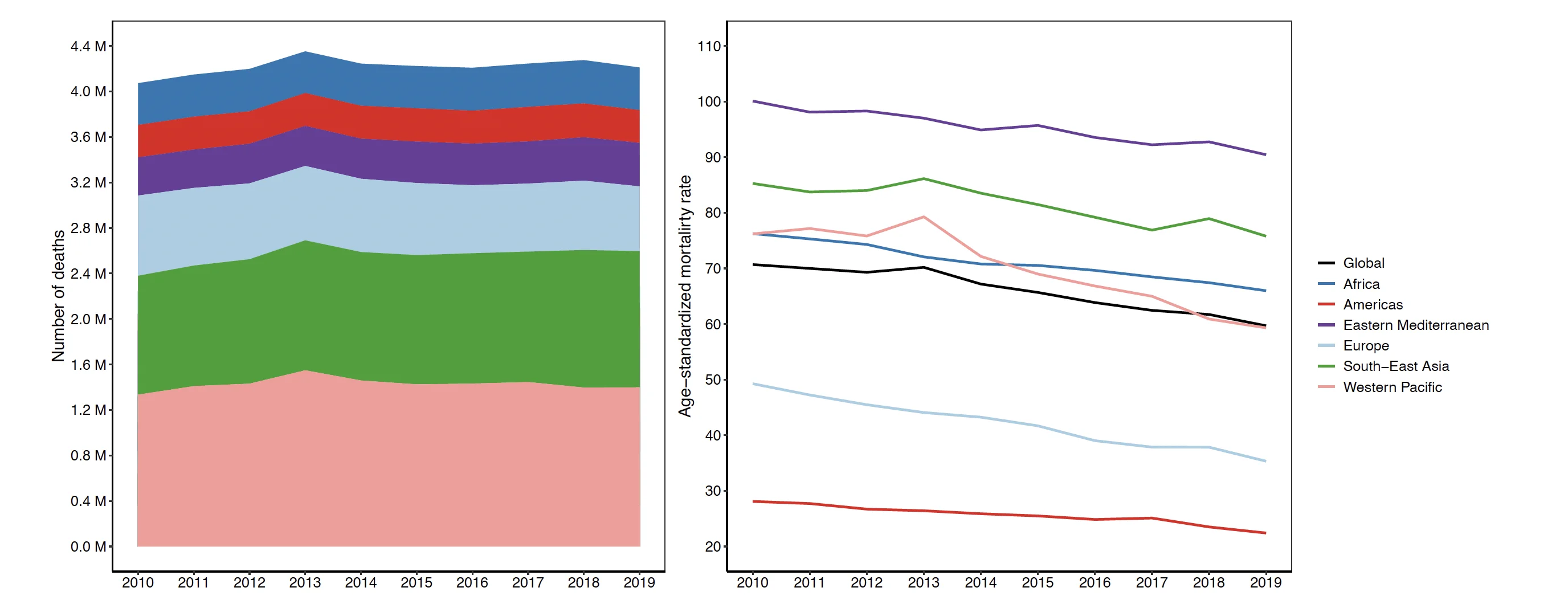
FIGURE 6 - Number of deaths (left panel) and age-standardized mortality rates (deaths per 100,000 people) (right panel) attributable to ambient air pollution for both sexes and WHO regions. Source: WHO Global Health Observatory
AMBIENT AIR POLLUTION AND CARDIOVASCULAR HEALTH
There is expansive literature linking air pollution to most cardiovascular conditions, with most studies run in high-income countries [13]. Limited data exists from LMICs. Cardiovascular conditions linked to air pollution include:
• IHD/Coronary artery disease
• Cerebrovascular disease
• Stroke
• Heart failure
• Cardiac arrhythmia and arrest
• Venous thromboembolism and peripheral artery disease such as pulmonary hypertension
• Dilated cardiomyopathy
• Congenital heart disease
• Pulmonary hypertension
CONSIDERABLE PROGRESS HAS BEEN MADE IN ESTABLISHING HOW AIR POLLUTION NEGATIVELY IMPACTS THE CARDIOVASCULAR SYSTEM*, WITH THE EFFECTS INCLUDING:
• Endothelial dysfunction
• The generation of oxidative stress
• Loss of endothelial-derived nitricoxide bioavailability
• Increases in circulating vasoconstrictive mediators
• Platelet activation
• Impaired fibrinolysis
• Endothelial cell inflammation
• Promotion of inflammatory pathways in endothelial cells
• Emerging evidence for pathways such as epigenetic modification, circulating microRNA and changes to circulating stem cell populations
Long-term exposure to air pollution has also been shown to accelerate atherosclerosis (narrowing of the arteries) and promote plaque instability.
*[14] (FIGURE 8)
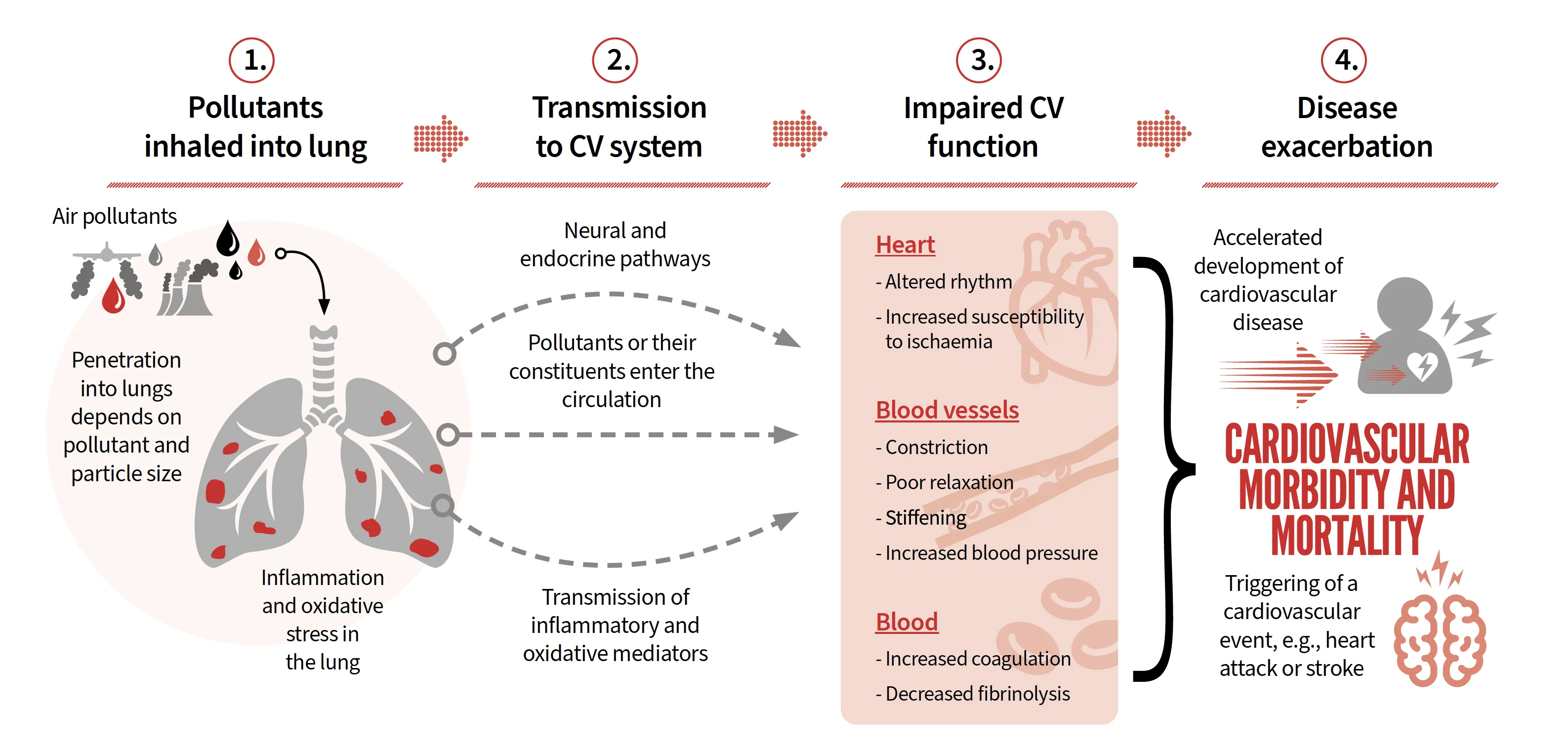
FIGURE 8 - Pathway by which air pollution leads to cardiovascular morbidity and mortality
MOST LARGE-SCALE META-ANALYSES SHOW CLEAR ASSOCIATIONS BETWEEN EXPOSURE TO BOTH SHORT-TERM AND LONG-TERM AIR POLLUTANTS AND THE INCREASED RISK OF CVDs.
READ MORE
In many cases, various CVDs are associated with more than one pollutant. While there will be some overlap in risk estimates from closely related pollutants, combined air pollutant mixtures will compound risks.
Read the full findings around the Household (indoor) air pollution and CVDs here.
CARDIOVASCULAR MORTALITY AND MORBIDITY ATTRIBUTABLE TO AMBIENT AIR POLLUTION
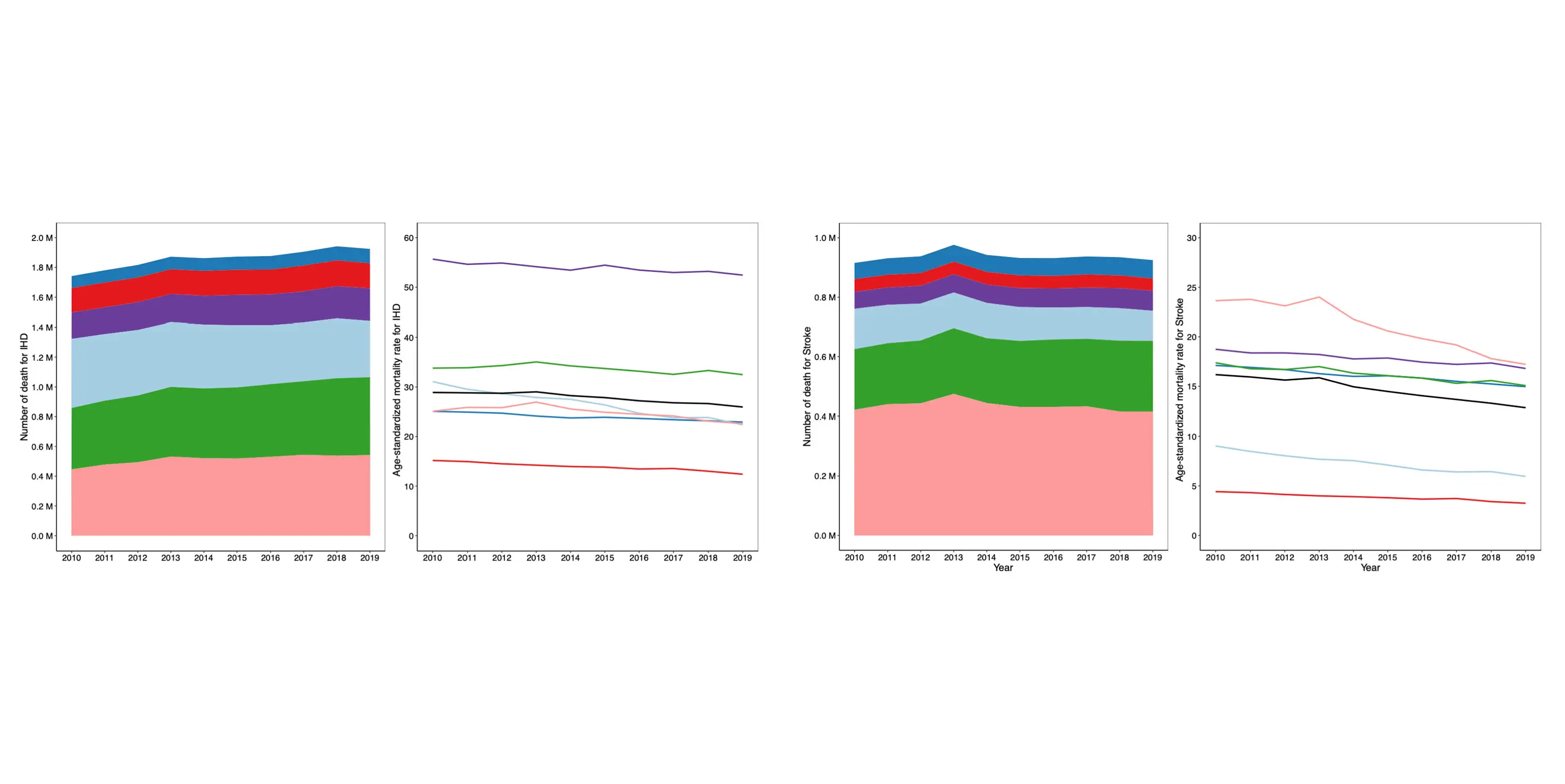
The global number of deaths from stroke attributable to air pollution increased only 1% from 2010 to 2019, though with significant regional variation. Increases were observed in the Africa, South-East Asia, and Eastern Mediterranean regions in this period, while Europe experienced a 25.3% decline, and the Americas and Western Pacific regions saw lesser reductions. Levels of age-standardized stroke mortality rates attributable to air pollution declined in all regions from 2010 to 2019, with the Eastern Mediterranean, Africa, and South-East Asia regions recording an average annual reduction of around 1%. The remaining regions experienced annual average reductions of 2.6-3.3% (Figure 11). There is no significant difference between males and females in the regional distribution of IHD deaths attributable to air pollution, except in the Europe region, where the proportion of female IHD deaths was higher (22.5%) than male deaths (17%) (Figure 12).
Regarding deaths from stroke attributable to air pollution, almost 50% of total global male deaths occurred in the Western Pacific, compared to 40% of total global female deaths. As with IHD, the proportion of female stroke mortality attributable to air pollution in the Europe region was higher than males (13.4% compared to 8.8%)*.
*Note that these burden estimates from an ecological study level would not capture differences in exposure to air pollution between genders arising from differences in behaviour and location throughout the day (i.e., air pollution exposure would be the same for males and females).
FIGURE 11 - Number of IHD and stroke deaths (left panels) and age-standardized mortality rates (per 100,000 people) (right panels) attributable to ambient air pollution for both sexes and WHO regions. Source: WHO Global Health Observatory
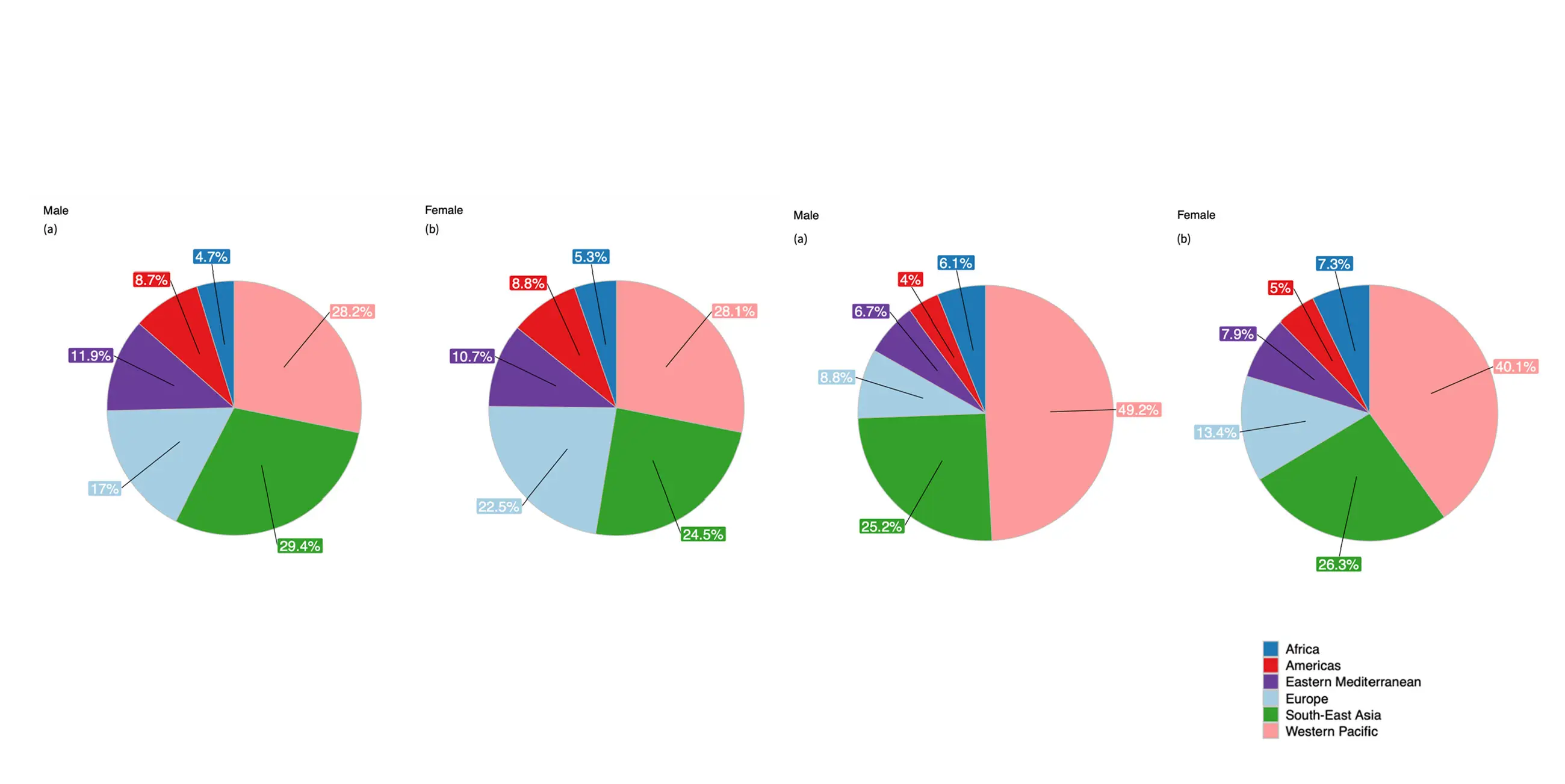
FIGURE 12 - Percentage of a) ischaemic heart disease and b) stroke mortality attributable to ambient air pollution by sex and WHO regions, 2019. Source: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/concentrations-of-fine-particulate-matter-(pm2-5)
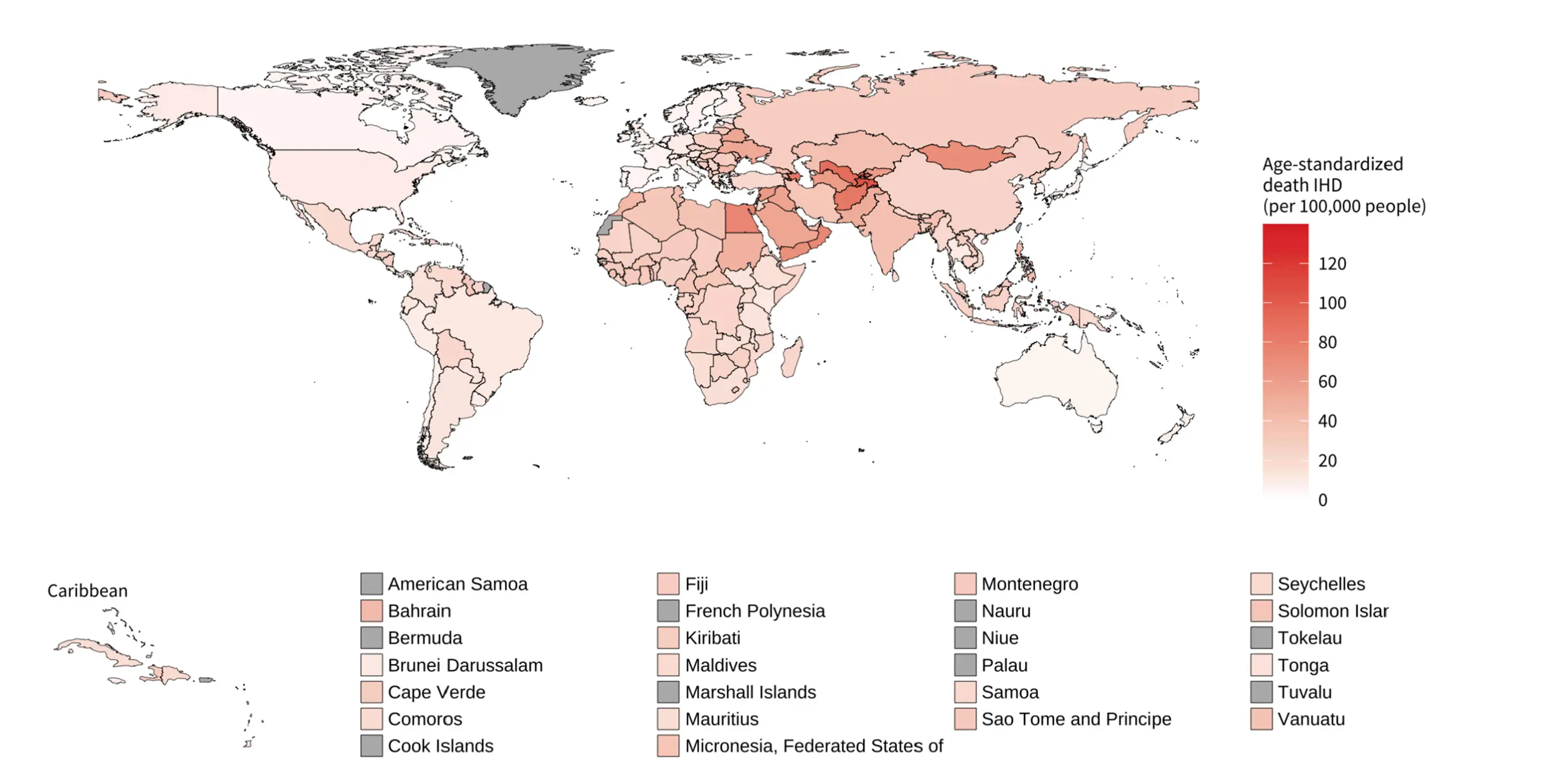
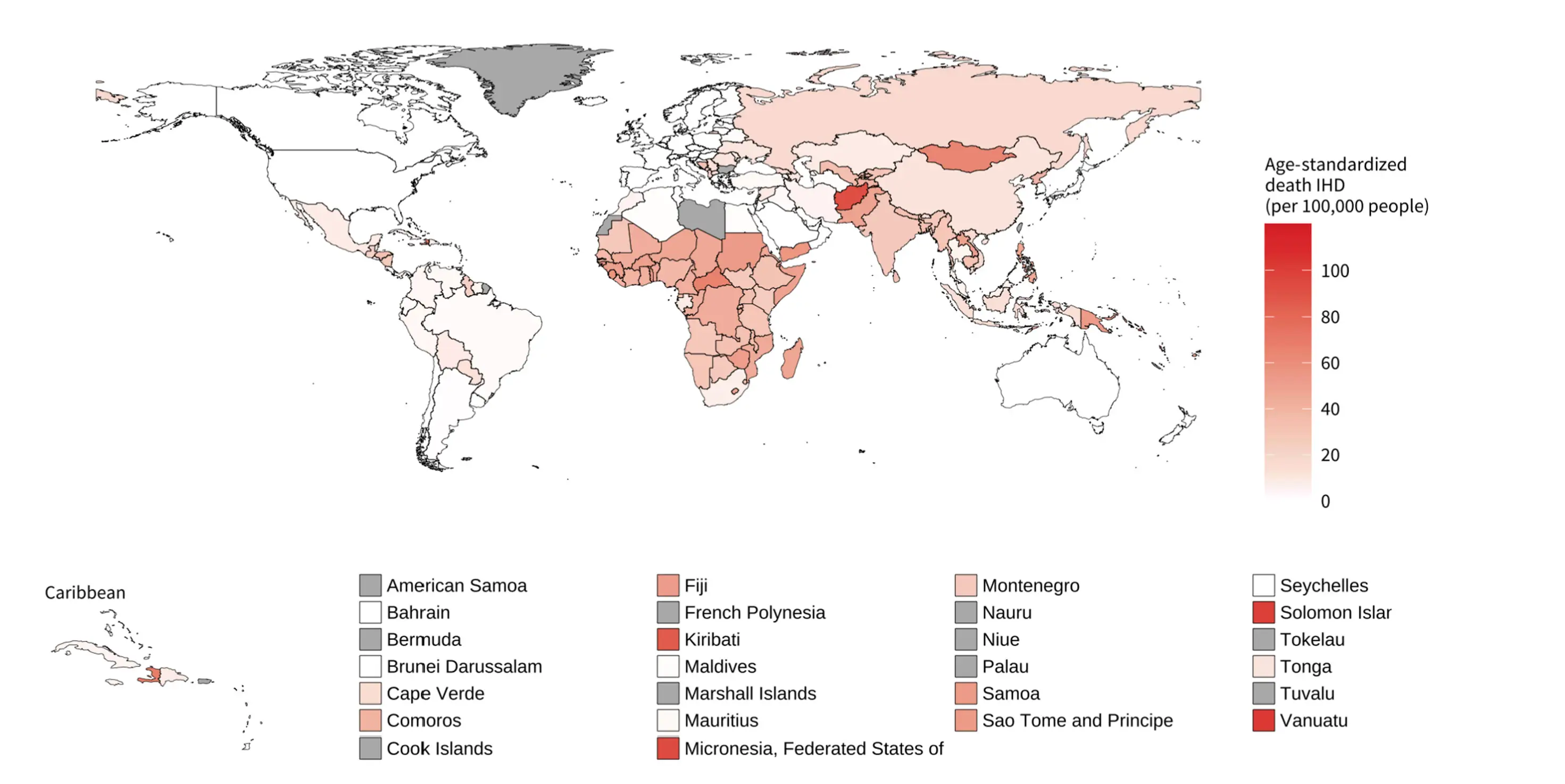
FIGURE 14 - Age-standardized ischaemic heart disease mortality rates (deaths per 100,000 people) attributable to ambient air pollution for both sexes, 2019 (WHO)
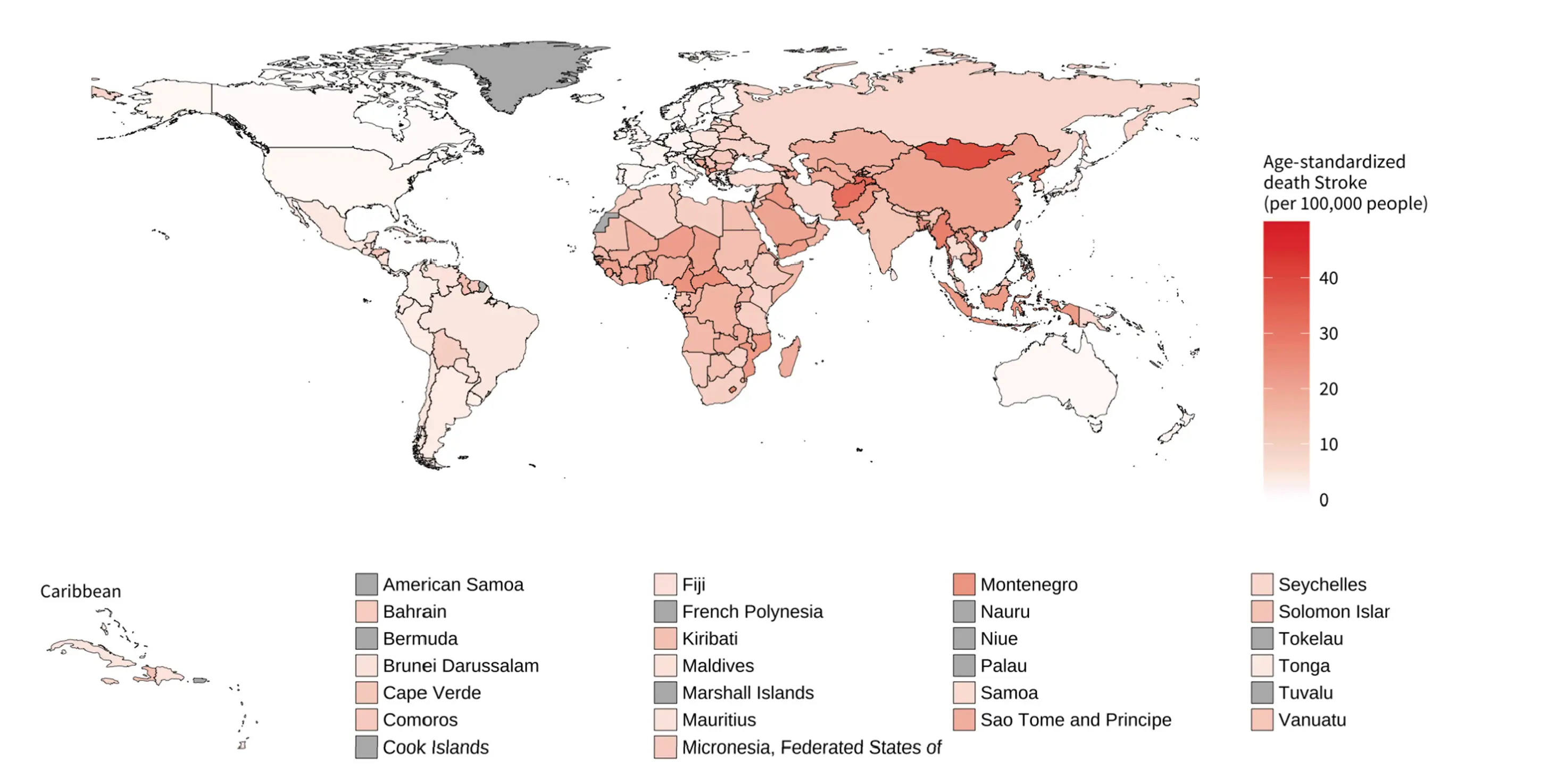
FIGURE 15 - Age-standardized stroke mortality rates (deaths per 100,000 people) attributable to ambient air pollution for both sexes, 2019 (WHO)
5. HOUSEHOLD (INDOOR) AIR POLLUTION AND CVDs

Exposure to household air pollution is among the top 10 risk factors for disease, with the poorest communities in LMICs most affected [1].
READ MORE
Estimates in 2019 showed that household air pollution contributed to 3.2 million deaths annually.
Over half of these 3.2 million deaths were due to cardiovascular disease, with 1 million from IHD and 700,000 from stroke.
In 2019, the three countries with the highest age-standardized IHD mortality attributable to household air pollution (deaths per 100,000 people) were Vanuatu (103 deaths; CI 79-126), Solomon Islands (100 deaths; CI 77-122) and the Federal State of Micronesia (94 deaths; CI 69-118). The lowest levels, outside of the high-income countries where no burden for household air pollution is estimated, were recorded in Argentina (0.3 deaths; CI 0.0-2.6), Jordan (0.4 deaths; CI 0.0-3.2) and Tunisia (0.8 deaths; CI 0.0-5.0) (Figure 17).
LMICs experience most of the burden, due to comparatively limited access to electricity or gas cooking.
In 2021, the proportion of the population with primary reliance on polluting fuels and technologies for cooking was highest in Africa (Sub-Saharan region), with South Sudan (100% of the population; CI 96. 1-100), Burundi (99.8%; CI 94.6-100), and Liberia (99.6%; CI 94.6-100) recording the highest values.
Read the full findings around the Household (indoor) air pollution and CVDs here.
GOVERNMENT INTERVENTION VIA POLICY AND TARGETED INVESTMENTS CAN ACCELERATE THE ADOPTION OF CLEAN COOKING SOLUTIONS AND HAS BEEN SUCCESSFUL IN COUNTRIES SUCH AS CHINA, INDIA, AND INDONESIA.
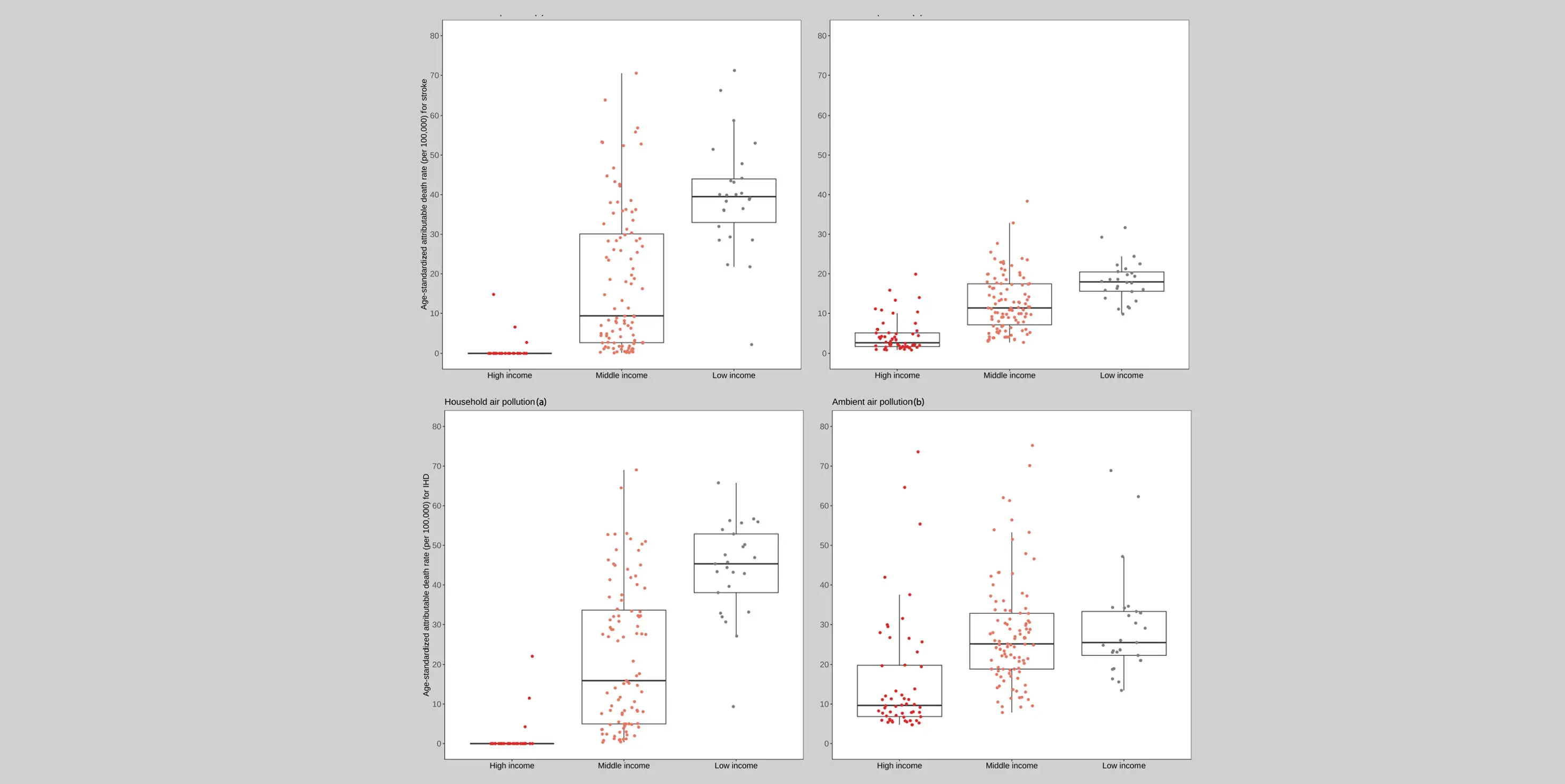
FIGURE 18 - IHD and stroke age-standardized mortality rates (deaths per 100,000 people) attributable to household air pollution(a) and ambient air pollution(b), by income level for both sexes, 2019. Source: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/ambient-air-pollution-attributable-death-rate-(per-100-000-population-age-standardized)
When countries are grouped by income level, the impacts of ambient (outdoor) and household (indoor) air pollution on people’s health differ significantly (Figure 18).
READ MORE
Countries in the low-income group experience higher levels of age-standardized stroke and IHD mortality attributable to both household and ambient air pollution than those in the middle- and high-income groups, with the exception of IHD mortality attributable to ambient air pollution. A larger gap is observed in levels of stroke and IHD mortality attributable to household air pollution, with most of the countries in the high-income group having no deaths attributable to household air pollution.
Read the full findings around the Household (indoor) air pollution and CVDs here.
COOKING AND HEATING CAN PRODUCE HIGH LEVELS OF POLLUTANTS WITH SPIKES IN POLLUTION OFTEN ORDERS OF MAGNITUDE HIGHER THAN AMBIENT LEVELS.
Certain groups and individuals are more susceptible to air pollution's negative health impacts, including pregnant people; those with lung or heart conditions; and those with obesity, hypertension, or diabetes.
PREGNANCY
Exposure to air pollution during pregnancy is linked with effects on the mother [22], including hypertensive disorders in pregnancy and gestational diabetes, and is associated with adverse birth outcomes such as pre-term birth, low birth weight and, in some settings, still-birth [23].
In utero exposure to air pollution has been linked to health effects in the child in later life, including the risk of developing CVDs.
OBESITY & DIABETES
Growing evidence shows that air pollution is linked with both obesity and diabetes. The exposure to air pollution is associated with impaired glucose handling, insulin resistance, as well as increased prevalence of diabetes and risk of death from diabetes due to long-term exposure to pollution.
Given the prevalence of cardiovascular conditions in patients with diabetes and obesity, the effects of air pollution in obese and diabetic individuals are likely to indirectly cause significant levels of morbidity and mortality.
HYPERTENSION
There is robust evidence that both short- and long-term exposure to air pollution increases blood pressure, the incidence and prevalence of hypertension, as well as hypertensive clinical events. The hypertensive effects of air pollution may contribute to associations between air pollution and other cardiovascular (and non-cardiovascular) conditions and events [27].
TOBACCO SMOKING
Air pollution is the second leading cause of death from non-communicable diseases (NCDs) after tobacco smoking [29]. Studies suggest that air pollution and smoking build on one another to have combined cardiovascular effects [30]. A substantial reduction in cardiovascular events—including beyond people who smoke—has been observed following the ban on cigarettes in public places in many countries [33], [34].
NOISE, LIGHT, TEMPERATURE AND MICROPLASTICS
It is estimated that 113 million people live in settings with levels of traffic noise that are harmful to health [36].
Exposure to noise has been associated with increases in the risk of cardiovascular mortality and morbidity, including IHD, heart failure, and stroke. A recent study identified nano-plastics in atherosclerotic plaques, which was associated with a higher risk of cardiovascular events and death [43].
MITIGATING AIR POLLUTION HARMS - PHYSICAL ACTIVITY
The global number of deaths from stroke attributable to air pollution increased only 1% from 2010 to 2019, though with significant regional variation. Increases were observed in the Africa, South-East Asia, and Eastern Mediterranean regions in this period, while Europe experienced a 25.3% decline, and the Americas and Western Pacific regions saw lesser reductions. Levels of age-standardized stroke mortality rates attributable to air pollution declined in all regions from 2010 to 2019, with the Eastern Mediterranean, Africa, and South-East Asia regions recording an average annual reduction of around 1%. The remaining regions experienced annual average reductions of 2.6-3.3% (Figure 11). There is no significant difference between males and females in the regional distribution of IHD deaths attributable to air pollution, except in the Europe region, where the proportion of female IHD deaths was higher (22.5%) than male deaths (17%) (Figure 12).
Regarding deaths from stroke attributable to air pollution, almost 50% of total global male deaths occurred in the Western Pacific, compared to 40% of total global female deaths. As with IHD, the proportion of female stroke mortality attributable to air pollution in the Europe region was higher than males (13.4% compared to 8.8%)*.
*Note that these burden estimates from an ecological study level would not capture differences in exposure to air pollution between genders arising from differences in behaviour and location throughout the day (i.e., air pollution exposure would be the same for males and females).

6. AIR POLLUTION AND CLIMATE CHANGE
Climate change and air pollution are interlinked. Most of the major drivers of air pollution, such as fossil fuel combustion and other anthropogenic activities, are also sources of greenhouse gas emissions, thereby driving climate change, while major environmental events caused by climate change increase air pollution, creating a vicious cycle [50].
READ MORE
Wildfire smoke has been linked toIHD, heart failure, and hospitalization for acute coronary events and stroke [54]. The increase in incidence, size, and severity of wildfires inrecent years has produced plumes of harmful air pollutants that can travel many kilometres from source. Climate changes have led to longer pollen seasons, with biological exposures like pollen and mould interacting with air pollutants to exacerbate allergic diseases.
Heat is often accompanied by stagnant weather, reducing the dissipation of air pollutants and promoting photochemical formation of other pollutants, such as ozone. Stagnant weather from temperature inversions can also result in episodes of cold temperature and air pollution, precipitating cardiovascular stress [56].
Read the full findings around Air pollution and climate change here.

TEMPERATURE, AIR POLLUTION, AND CVDs
CVDs can be attributed to extreme temperatures. Temperature and air pollution have been shown to each enhance the impacts of the other [58].
INDIRECT IMPACTS OF CLIMATE CHANGE
Air pollution has health inequities both in terms of the level of exposure (with those of lower socio-economic status likely to have higher exposure) and effect (with those that are already vulnerable being more biologically susceptible to the effects of pollutant exposure).
Because they are closely interconnected, mitigation and other interventions targeting and tackling air pollution have the co-benefit of acting on climate change [60].
There is a need to be cautious that policies and interventions to tackle one environmental risk do not have inadvertent consequences on another.
7. AIR QUALITY GUIDELINES AND POLICIES

National and local governments have a critical role to play in reducing air pollution through policy implementation. The 2021 WHO Global Air Quality Guidelines provide policymakers with recommended levels for air pollutants based on the evidence of their impact on health, along with interim targets to guide progress towards recommended levels.
READ MORE
At the city level, these include steps to reduce emissions from vehicles through traffic charging and parking policies, improved public transport and infrastructure for cycling and walking, zoning laws to prevent residential zones from being near areas with industrial and traffic activity, updated building codes to require indoor air filtration and reduce penetration of ambient air pollution, advisory and prevention monitoring to notify communities if pollutants are exceeding safe levels, fossil fuel taxes, and penalties for excessive air pollution [62].
At the national level, governments can provide policy support and legal frameworks for the implementation of more local policies. This includes national legislation and engagement with global mechanisms related to setting and monitoring air pollution standards and commitments, such as the 2015 Paris Climate Agreement and the annual World Health Assembly.
122 countries plus the EU (64%) have legislation or policy/guideline documents empowered under law, which contain ambient air quality standards (AAQS) [63]. Most countries without AAQS legislation are in the Africa region (Figure 20).
Read the full findings around Air quality guidelines and policies here.
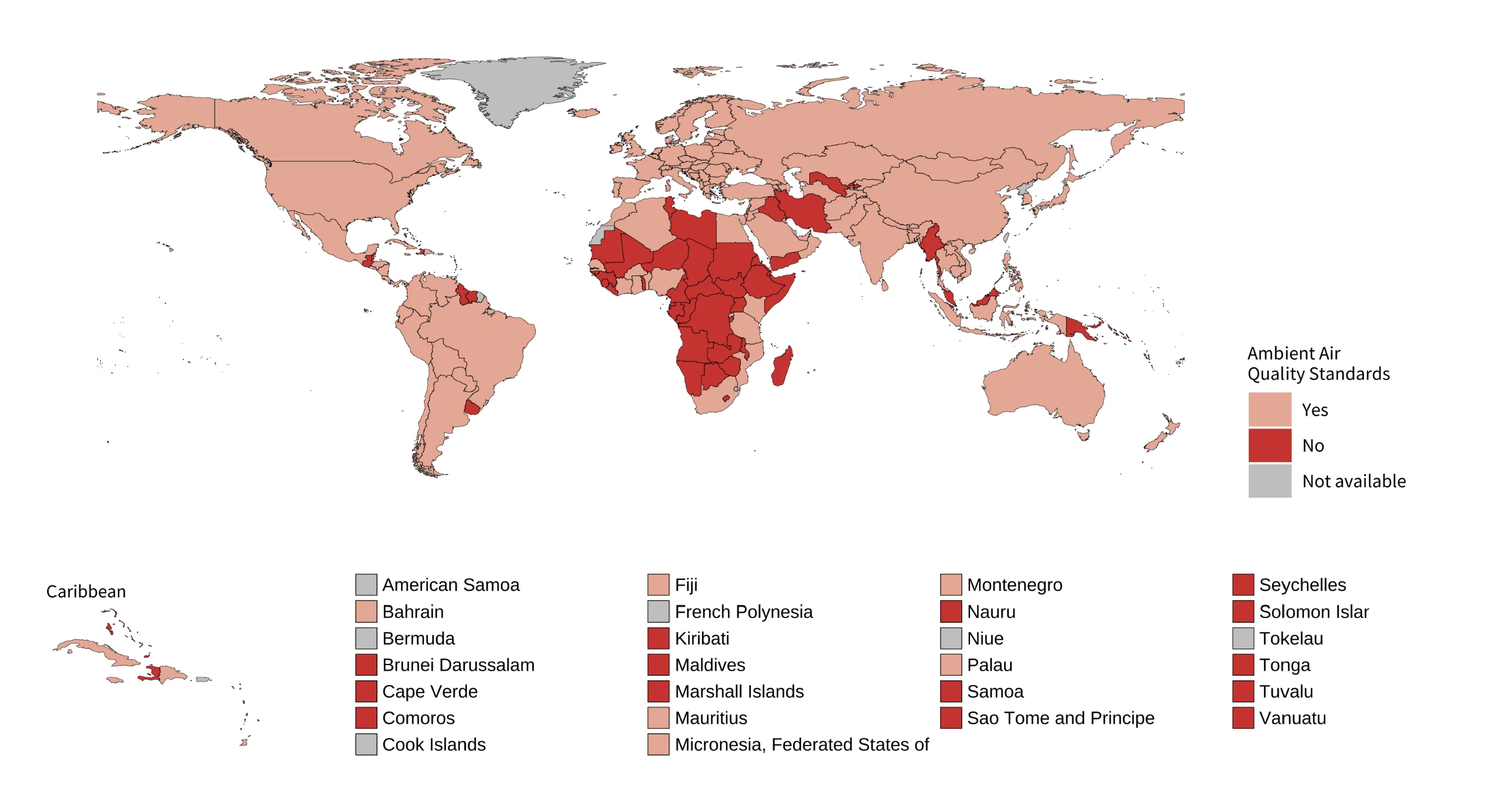
FIGURE 20 - Countries with legal instruments containing Ambient Air Quality Standards. Figure reproduced from: https://www.unep.org/resources/report/regulating-air-quality-first-global-assessment-air-pollution-legislation
READ MORE
The proportion of countries with legal requirements to monitor air quality is similarly limited at only 57%. Europe is the only region where a notable majority of countries have a requirement to monitor air quality incorporated into law (95%). The Americas (53%) and Eastern Mediterranean (50%) are the only other regions with half or more of countries having such legislation, with Africa (30%) having the lowest proportion of countries with a legal requirement for monitoring.
Overall, less than a third of analysed Nationally Determined Contributions (NDCs) referred to the health impacts of air pollution. There is also a need for stronger policies and commitments from governments and multilateral bodies to increase funding for research, technical innovations, and implementation projects to tackle air pollution. Less than 2% of international development funds, philanthropic foundation funding, and international public climate finance went to tackle air pollution between 2015 and 2021.
Read the full findings around Air quality guidelines and policies here.

AGRICULTURE POLICIES
Agriculture is a significant source of air pollution.
Methods to reduce ammonia emissions from agricultural practices already exist (e.g., urease inhibitors in fertilizer, slurry store covers, fertilizer injection, and lower protein animal feeds).
However, farmers across the world already increasingly work on narrow economic margins and pressures from bureaucratic administration. Another source of agricultural-derived emissions, especially in LMICs, is from crop and stubble burning. Plumes from agricultural biomass burning are significant and can travel long distances, contributing to the PM levels in neighbouring countries [73]. The cardiovascular effects of agriculture-derived emissions, especially secondary PM from ammonia, are yet to be established. An understanding of the contribution of agricultural PM to CVDs would provide scientific support to accelerate policy change.

VEHICLE STANDARDS
Many countries have legislation and annual checking for vehicle standards to ensure safety, and the inclusion and extent of emission testing are growing.
Progress has been made in reducing tailpipe emissions from new vehicles, both in terms of NO2 and particulates, even in modern diesel engines where emissions are becoming comparable to that of gasoline engines. And while modern vehicle engines are substantially cleaner than their counterparts a decade ago, the average vehicle age is around 10 years old in European nations, considerably older in LMICs. The installation of "particle filters" on vehicle exhaust has been a factor in reducing PM emissions from newer vehicles, yet compliance to maintain (or even retain) these filters is mixed [76]. Vehicle exhaust is also the major source of harmful ultra-fine particles in urban areas. As the world slowly moves away from the combustion engine to cleaner technologies such as electric vehicles, the proportion of non-exhaust emissions from traffic will increase. Developing the legislation on non-exhaust emissions will be important over the forthcoming decades, and the passion for technological innovation in this area is reassuring. Ultimately, though, cardiovascular effects remain woefully under-explored.

Provision of clean domestic fuels
Indoor air pollution is associated with significant levels of morbidity and mortality, including through CVDs (see section on Household Pollution and CVDs). Solid-fuel use drives this burden in LMICs, with domestic exposure to combustion-derived PM and gases especially high during cooking and home heating [78]. In low-income regions, single-room housing may lead to prolonged exposure to pollutants where ventilation is not considered, especially for women who tend to have greater exposure to cooking fumes in LMICs. A move from solid fuel combustion to the use of LPG and solar panels is urgently needed in LMICs, with use of clean stove combustion advisable where clean fuel options are not available. There are examples of clean fuel initiatives in many countries, such as the World Bank-supported Bangladesh Improved Cookstove Programme. This used a market model to help 3.4 million people gain access to improved cooking solutions while creating 3,000 jobs and saving 3.54 million tons of biomass fuel annually [79]. Successful programmes such as the one in Bangladesh will be helpful in guiding and expanding other programmes. It is important that governments, local bodies, and international partners provide the necessary support, financially, logistically and through legislation, to make clean fuel provision universal.

URBAN PLANNING AND INFRASTRUCTURE
Over 50% of the world’s population lives in cities [80].
Better housing may reduce the ingress of ambient air pollution into indoor spaces, and ventilation can be optimized to reduce egress of indoor air pollutants out of the home [81].
The transition to “20-minute neighbourhoods”, where necessary amenities can be reached from a residence within 20 minutes without taking a private vehicle, will take considerable time and resources to achieve; however, policies are moving in this direction, with cities including Bogotá, Melbourne, Milan, Paris, and Portland cited as good practice examples [84]. The gradual move towards healthy cities will be rewarded through gains in physical and mental health, as well as economic and environmental sustainability [85].
ENVIRONMENTAL INJUSTICE IS THE INEQUITABLE AND DISPROPORTIONATE EXPOSURE OF POOR, RACIAL AND ETHNIC MINORITIES, AND DISENFRANCHISED POPULATIONS TO TOXIC CHEMICALS, AIR AND WATER POLLUTION, UNSAFE WORKPLACES, AND OTHER ENVIRONMENTAL HAZARDS.
READ MORE
The idea of environmental injustice is correlated with the unequal exposure to pollution, and other factors linked to poverty, such as inadequate access to medical and preventive care and other conditions like malnutrition or the lack of pollution healthcare in the workplace [87]. In LMICs, heating and cooking by biomass and the relocation of polluting industries from high-income countries are emblematic of the disparities in air pollution exposure [88]. These are examples of environmental justice conflicts involving air pollution that can be found on every continent, with the majority most likely to have a greater impact on vulnerable populations with little capacity to enforce their rights.
Read the full findings around Air quality guidelines and policies here.
8. KEY RECOMMENDATIONS

All countries and stakeholders must urgently work together to accelerate efforts to curb air pollution levels and implement policy and health interventions to protect people from its most harmful effects. These actions will be critical to achieving Sustainable Development Goals related to cutting non-communicable disease mortality, as well as having broader benefits with regard to tackling the climate crisis.
1
WHF encourages the healthcare sector to take a leading stance in reducing emissions of air pollution as part of sustainability strategies. Currently, the healthcare sector accounts for almost 5% of global greenhouse gas emissions.
2
WHF encourages cardiologists, cardiovascular scientists, health practitioners in general, cardiovascular communities and health foundations to advocate for the need to recognize air pollution as a major risk factor for cardiovascular health, engage with stakeholders, and help prioritize resources and political will to tackle this issue.
3
Greater efforts must be made to improve education on the health impacts of air pollution, including at secondary, undergraduate, and postgraduate levels, for health professionals and through training programmes for disciplines essential for research in the field, e.g., toxicology and epidemiology.
4
More studies on the cardiovascular effects of air pollution are required in LMICs.
BIBLIOGRAPHY
1. Institute for Health Metrics and Evaluation. VizHub - GBD Compare [Internet]. [cited 2024 Apr 25]. Available from: https://vizhub.healthdata.org/gbd-compare/
2. World Bank. The Global Health Cost of PM2.5 Air Pollution: A Case for Action Beyond 2021 [Internet]. International Development in Focus. The World Bank; 2022. 86 p. Available from: https://doi.org/10.1596/978-1-4648-1816-5
3. OECD. The Economic Consequences of Outdoor Air Pollution. The Economic Consequences of Outdoor Air Pollution. 2016 Jun 9
11. Schraufnagel DE, Balmes JR, Cowl CT, De Matteis S, Jung SH, Mortimer K, et al. Air Pollution and Noncommunicable Diseases: A Review by the Forum of International Respiratory Societies 2019; Environmental Committee, Part 2: Air Pollution and Organ Systems. Chest. 2019 Feb 1;155(2):417–26. Available from: https://doi.org/10.1016/j.chest.2018.10.041
13. de Bont J, Jaganathan S, Dahlquist M, Persson Å, Stafoggia M, Ljungman P. Ambient air pollution and cardiovascular diseases: An umbrella review of systematic reviews and meta-analyses. J Intern Med. 2022 Jun 1;291(6):779–800. Available from: https://doi.org/10.1111/joim.13467
14. Miller MR, Newby DE. Air pollution and cardiovascular disease: car sick. Cardiovasc Res. 2020 Feb 1;116(2):279-294. doi: 10.1093/cvr/cvz228. PMID: 31583404.
21. Zhao B, Zheng H, Wang S, Smith KR, Lu X, Aunan K, et al. Change in household fuels dominates the decrease in PM2.5 exposure and premature mortality in China in 2005–2015. Proceedings of the National Academy of Sciences. 2018 Dec 4;115(49):12401–6. Available from: https://doi.org/10.1073/pnas.1812955115
22. Decrue F, Townsend R, Miller MR, Newby DE, Reynolds RM. Ambient air pollution and maternal cardiovascular health in pregnancy. Heart. 2023 Nov 1;109(21):1586. Available from: http://heart.bmj.com/content/109/21/1586.abstract
23. Klepac P, Locatelli I, Korošec S, Künzli N, Kukec A. Ambient air pollution and pregnancy outcomes: A comprehensive review and identification of environmental public health challenges. Environ Res. 2018 Nov;167:144–59
27. Giorgini P, Di Giosia P, Grassi D, Rubenfire M, D. Brook R, Ferri C. Air Pollution Exposure and Blood Pressure: An Updated Review of the Literature. Curr Pharm Des. 2015 Dec 21;22(1):28–51.
29. World Health Organization. Noncommunicable diseases and air pollution [Internet]. [cited 2024 Apr 26]. Available from: https://www.who.int/europe/news/item/29-03-2019-noncommunicable-diseases-and-air-pollution
30. Turner MC, Cohen A, Burnett RT, Jerrett M, Diver WR, Gapstur SM, et al. Interactions between cigarette smoking and ambient PM 2.5 for cardiovascular mortality. Environ Res. 2017 Apr;154:304–10.
33. Pell JP, Haw S, Cobbe S, Newby DE, Pell ACH, Fischbacher C, et al. Smoke-free Legislation and Hospitalizations for Acute Coronary Syndrome. New England Journal of Medicine. 2008 Jul 31;359(5):482–91.
34. Xiao H, Zhang H, Wang D, Shen C, Xu Z, Zhang Y, et al. Impact of smoke-free legislation on acute myocardial infarction and stroke mortality: Tianjin, China, 2007–2015. Tob Control. 2020 Jan;29(1):61–7.
36. European Environment Agency. 2020. [cited 2024 Apr 26]. Environmental noise in Europe — 2020. Available from: https://www.eea.europa.eu/publications/environmental-noise-in-europe
43. Marfella R, Prattichizzo F, Sardu C, Fulgenzi G, Graciotti L, Spadoni T, et al. Microplastics and Nanoplastics in Atheromas and Cardiovascular Events. New England Journal of Medicine. 2024 Mar 7;390(10):900–10.
50. United Nations Environment Programme. Air pollution and climate change: two sides of the same coin [Internet]. [cited 2024 Apr 29]. Available from: https://www.unep.org/news-and-stories/story/air-pollution-and-climate-change-two-sides-same-coin
54. Miller M, et al. Pollution and Cardiovascular Disease, Part 1: Global Warming, Air Pollution and Wildfires. Journal of the American College of Cardiology, in press. 2024
56. Li J, Woodward A, Hou XY, Zhu T, Zhang J, Brown H, et al. Modification of the effects of air pollutants on mortality by temperature: A systematic review and meta-analysis. Science of The Total Environment. 2017 Jan;575:1556–70.
58. Anenberg SC, Haines S, Wang E, Nassikas N, Kinney PL. Synergistic health effects of air pollution, temperature, and pollen exposure: a systematic review of epidemiological evidence. Environ Health. 2020 Dec 1 [cited 2024 Apr 29];19(1):1–19. Available from: https://link.springer.com/articles/10.1186/s12940-020-00681-z
60. Haines A. Health co-benefits of climate action. Lancet Planet Health. 2017 Apr;1(1):e4–5.
62. World Heart Federation. Clean Air, Smart Cities, Healthy Hearts: Action On Air Pollution For Cardiovascular Health - A World Heart Federation Policy Brief. [cited 2024 Apr 25]; Available from: https://world-heart-federation.org/resource/clean-air-smart-cities-healthy-hearts-a-whf-policy-brief/
63. United Nations Environment Programme. Regulating Air Quality: The first global assessment of air pollution legislation [Internet]. Nairobi; 2021 [cited 2024 May 8]. Available from: https://www.unep.org/resources/report/regulating-air-quality-first-global-assessment-air-pollution-legislation
73. Asian Development Bank Blog by Yoko Watanabe YS. A Burning Issue: Managing Air Quality in Cities and Rural Areas [Internet]. 2024 [cited 2024 May 8]. Available from: https://blogs.adb.org/blog/burning-issue-managing-air-quality-cities-and-rural-areas
76. United States Environmental Protection Agency. Aftermarket Defeat Devices and Tampering are Illegal and Undermine Vehicle Emissions Controls. 2020 [cited 2024 Apr 29]; Available from: https://www.epa.gov/sites/default/files/2020-12/documents/tamperinganddefeatdevices-enfalert.pdf
78. World Health Organization. Equity impacts of air pollution [Internet]. 2014 [cited 2024 May 8]. Available from: https://www.who.int/teams/environment-climate-change-and-health/air-quality-and-health/health-impacts/equity-impacts
79. World Bank Energy Sector Management Assistance Programme. MPACT Newsletter, Issue 17 [Internet]. 2019 [cited 2024 May 8]. Available from: https://www.worldbank.org/en/results/2023/01/19/moving-the-needle-on-clean-cooking-for-all
80. World Bank. Urban Development Overview [Internet]. 2023 [cited 2024 May 8]. Available from: https://www.worldbank.org/en/topic/urbandevelopment/overview
81. World Health Organization. Strategies for reducing exposure household air pollution include clean fuels and stoves, supportive policies and awareness-raising campaigns [Internet]. [cited 2024 May 8]. Available from: https://www.who.int/teams/environment-climate-change-and-health/air-quality-energy-and-health/sectoral-interventions/household-air-pollution/strategies
84. C40 Knowledge Hub. Benchmark: 15-minute cities [Internet]. [cited 2024 May 8]. Available from: https://www.c40knowledgehub.org/s/article/Benchmark-15-minute-cities
85. Rajagopalan S, Ramaswami A, Bhatnagar A, Brook RD, Fenton M, Gardner C, et al. Toward Heart-Healthy and Sustainable Cities: A Policy Statement From the American Heart Association. Circulation. 2024 Apr 9;149(15).
87. Rentschler J, Leonova N. Global air pollution exposure and poverty. Nat Commun. 2023 Jul 22;14(1):4432.
88. Adekoya A, Tyagi SK, Duru CN, Satia I, Paudyal V, Kurmi OP. Effects of Household Air Pollution (HAP) on Cardiovascular Diseases in Low- and Middle-Income Countries (LMICs): A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2022 Jul 29;19(15):9298.