WORLD HEART REPORT 2025
OBESITY & CARDIOVASCULAR DISEASE
1. EXECUTIVE SUMMARY

ONCE CONSIDERED AN ISSUE CONFINED TO HIGH-INCOME COUNTRIES, OBESITY IS NOW A FAST-INCREASING CHALLENGE FOR NEARLY EVERY COUNTRY OF THE WORLD, WITH PERVASIVE ECONOMIC AND HEALTH IMPACTS, PARTICULARLY AS IT RELATES TO THE WORLD’S BIGGEST KILLER — CARDIOVASCULAR DISEASE (CVD).
In 2022, 878 million adults lived with obesity, a quadrupling of the 194 million who lived with the disease in 1990. If the current growth trends continue, it is projected that nearly 2 in 3 adults aged 25 years or older could live with overweight or obesity by 2050.
READ MORE
Costs to the global economy from obesity-related healthcare needs, productivity losses and death are estimated to amount to 2.2% of global Gross Domestic Product (GDP) (just under US$2 trillion per year) and could reach 3% annually by 2060. Low- and middle-income countries (LMICs) and their health systems are set to bear the brunt of these impacts, though almost all countries will be affected.
In health terms, high Body Mass Index (BMI) causes 3.7 million deaths per year and are leading drivers of deaths from CVD. For example, annual global deaths from CVD attributable to high BMI more than doubled to 1.9 million in three decades, and high BMI now account for nearly 1 in 10 of all CVD deaths. That proportion is increasing in all but two regions of the world. The prevalence of obesity and the number of CVD deaths attributed to the disease vary by country, region, age and sex.
Crucial to efforts in tackling obesity and CVD is the need for a holistic approach across clinical and public health interventions that accounts for the myriad determinants of obesity. The role of these complex, interconnected factors underscores that obesity is far from being an individual choice. Determinants include environmental (access to exercise and green space), biological (genetic predisposition toward obesity), socioeconomic status (income, education and occupation), and commercial (policies/ regulations that address food marketing and affordability), among others.
Positive steps have been taken in recent years, with the implementation of several global, national, and local initiatives that show promise in tackling obesity and CVDs, in addition to the emergence of potentially gamechanging medical interventions, such as glucagon-like peptide-1 receptor agonists (GLP-1RAs).
The World Heart Federation (WHF)—with its membership of more than 200 heart foundations, scientific societies, and patient organisations across more than 100 countries—is committed to working with all stakeholders to urgently reduce obesity and CVDs. To support efforts, this report provides the following key recommendations:
Public health interventions
1
Countries should implement evidence-based and cost-effective public health measures to address obesity and CVD, drawing on global frameworks and tools. Countries should also prioritise comprehensive, integrated, and equity-focused policies guided by national data on how determinants vary across population groups. Priority actions include national obesity roadmaps with defined targets, multisectoral policies addressing the broad scope of obesity determinants, and ensuring greater integration of obesity prevention and treatment into primary healthcare services.
2
Public health campaigns and policies must counteract the stigmatization of obesity through using person-first language, recognising that stigma is a hindrance to tackling obesity and CVD, and should also involve people living with obesity and CVDs.
CLINICAL interventions
1
Cardiovascular guidelines should incorporate obesity-specific recommendations to ensure CVD management is adequately adapted for people living with obesity. This includes equipping health professionals with the knowledge, guidance and tools necessary to optimally prevent, manage and treat obesity.
2
Health professional education and health system strengthening initiatives for obesity and CVD should focus on promoting person-centred, integrated care and where possible be responsive to disparities in obesity risk, prevalence and access to care.
3
Governments should increase efforts to expand the availability and affordability of obesity medications, such as GLP-1RAs. Governments should increase efforts to expand the public awareness, availability, and accessibility of specialized lifestyle modification programmes, such as nutrition, physical activity, weight loss, and cardiac rehabilitation programmes.
2. INTRODUCTION

Image credit: © World Obesity
OBESITY IS WELL ESTABLISHED AS A MAJOR CONTRIBUTING FACTOR TO THE RISK OF CVD — A GROUP OF DISORDERS THAT AFFECT THE HEART, BLOOD VESSELS, AND BLOOD — WITH MULTIPLE OBESITY-RELATED MECHANISMS UNDERPINNING THE DEVELOPMENT OF CVD AND LEADING TO INCREASED MORBIDITY AND MORTALITY.
Along with providing a comprehensive overview and analysis of the latest available data, this report aims to equip advocates, policymakers, and clinicians with the information they need to inform interventions that will help urgently reduce the burden of obesity and CVD.
The report uses the latest comprehensive data sources available that are disaggregated by country, age and sex2,5 (see Online Appendix).
3. OVERWEIGHT, OBESITY AND CVD

Image credit: © World Obesity
OBESITY—THE EXISTENCE OF EXCESSIVE BODY FAT (ADIPOSITY)—IS A MAJOR PUBLIC HEALTH ISSUE THAT HINDERS SOCIAL DEVELOPMENT AND ECONOMIC PROGRESS1. IN ADDITION TO BEING A DISEASE ITSELF, OBESITY IS A RISK FACTOR FOR MANY NONCOMMUNICABLE DISEASES (NCDS), INCLUDING CVD, TYPE 2 DIABETES AND SEVERAL CANCERS.
READ MORE
The WHO defines obesity in adults (aged 18 years or older) as having a BMI of 30 kg/m² or more, and overweight as a BMI of 25–29.9 kg/m². In children below the age of 5 years, overweight and obesity are defined respectively as weight-for-height >2 and weight-for-height >3 standard deviations above the WHO Child Growth Standards median, while in children aged 5–19 years, overweight and obesity are respectively defined as a BMI-for-age >1 and BMI-for-age >2 standard deviations above the WHO Growth Reference median6.
While there are limitations associated with using BMI as a diagnostic tool for obesity and overweight in clinical practice (see section on the limitations of using BMI to define and diagnose obesity), it remains among the most useful, simple, and accessible indicators for disease surveillance, research studies, and estimating obesity at a population level. Consequently, the data in this report relies on BMI as a measure of obesity.
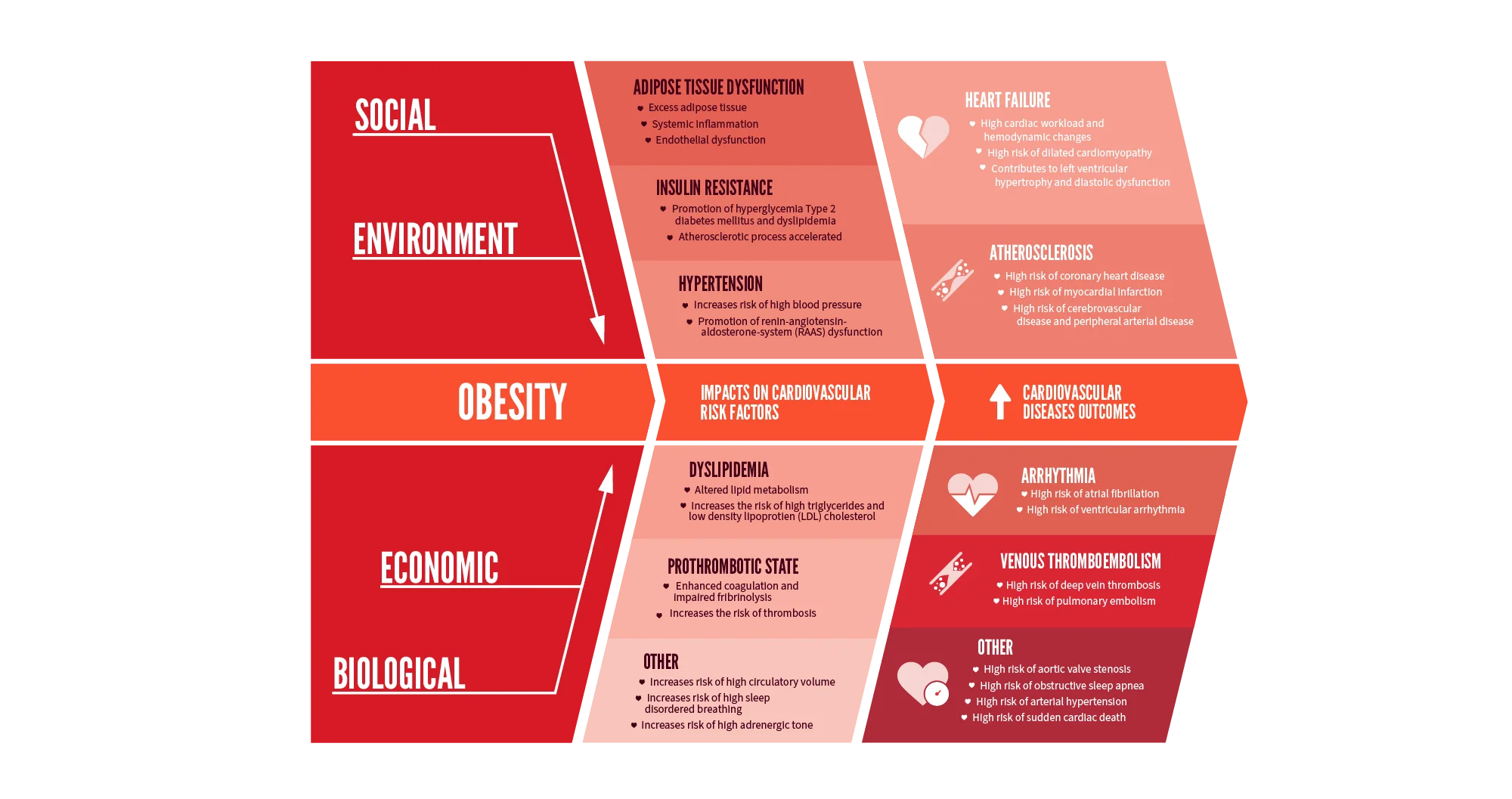
OBESITY IMPACTS SEVERAL CARDIOVASCULAR RISK FACTORS AND SUBSEQUENT CVD OUTCOMES THROUGH COMPLEX MECHANISMS (SEE FIGURE 1).
These include the development of risk factors, such as insulin resistance, adipose tissue dysfunction and dyslipidaemia, which contribute to the exacerbation of CVD outcomes, such as coronary heart disease, heart failure, myocardial infarction and thromboembolisms.
SHORT- AND LONG-TERM EFFECTS OF CHILDHOOD OBESITY ON CVDs
Over the past three decades, childhood obesity rates have increased dramatically across the globe. The age-standardized prevalence of obesity in school-aged children and adolescents (aged 5–19 years) increased from 1.7% in 1990 to 6.9% in 2022 for girls and from 2.1% to 9.3% for boys. Globally, the number of girls and boys with obesity in 2022 was 65.1 million and 94.2 million respectively.
READ MORE
Childhood obesity significantly increases cardiovascular risk, particularly for atherosclerotic cardiovascular disease, and the clustering of metabolic risk factors. These factors often include at least a two-fold increased odds of elevated blood pressure, abnormal lipid profiles, and Type 2 diabetes, establishing an adverse cardiovascular risk profile well before adulthood16.
In the short term, children living with overweight or obesity have more metabolic and cardiovascular risk factors, such as high blood pressure12, dyslipidemia13, Type 2 diabetes14, and other abnormalities of the cardiovascular system15. In the long term, if obesity or overweight is not addressed in childhood, then the short term metabolic and cardiovascular risk factors significantly increase the risk of developing CVDs in later life. For example, children with a high BMI are 40% more likely than those with a low BMI to suffer from CVD in midlife17. Children with a combination of risk factors, including smoking, high BMI, blood pressure and blood lipids have a two- to nine-fold greater risk of heart attack and stroke in midlife17.
The onset of obesity, especially at younger ages, has a profound negative effect on life expectancy, and can reduce it by as much as half of the average lifespan18. Interventions, including structured dietary and physical activity programmes, show a reduction in cardiometabolic risk factors, with potential long-term benefits if sustained19.
COMBATING MISCONCEPTIONS ABOUT OBESITY

MISCONCEPTION 1:
OBESITY RESULTS FROM AN IMBALANCE BETWEEN CALORIE INTAKE AND EXPENDITURE
The narrative around obesity has long centred around the over-simplified equation of “calories consumed - calories burnt = body weight.” However, the reality is more complex. Energy consumed is determined by both the quantity of food and the amount of food-derived energy that the gastrointestinal tract absorbs. This absorption is dependent on several factors, including digestive enzymes, gut hormones, microbiota and neural signals, all of which are beyond the control of the individual. Similarly, energy expended is not only dependent on physical activity, but also an individual’s metabolic rate, which accounts for 60–80% of the total daily expenditure65.
MISCONCEPTION 2:
OBESITY IS A LIFESTYLE CHOICE
People with obesity often face accusations of their disease being a personal choice, or that weight gain is due to a sedentary lifestyle and over-eating. The reality is more nuanced. Robust evidence exists linking obesity in most cases to social, biological, environmental, and commercial determinants, among others, (see section on Determinants of obesity and CVD).
MISCONCEPTION 3:
OBESITY IS NOT A DISEASE
Defining a disease requires empirical and objective, medical and biological evidence. Many people living with obesity meet these criteria, including specific symptoms or signs (e.g., increased adiposity), reduced life quality, increased risk of related complications, or well characterized pathophysiology (e.g., inflammation, endothelial dysfunction, insulin resistance, alterations in hormones regulating satiety or hunger).
The WHO and the WHF (through the 2015 Nagoya Declaration) and many other leading international and national bodies define obesity as a disease or disease process68,32.
4. GLOBAL LEVELS AND TRENDS OF OBESITY

In 2022, it was estimated that more than 1 billion people—878 million adults (over the age of 20 years) and 159 million children and adolescents—were living with obesity worldwide2. There were 504 million women and 374 million men with obesity respectively.
IN 2021, 3.7 MILLION DEATHS AND 128.5 MILLION DISABILITY-ADJUSTED LIFE YEARS (DALYs) WERE LOST DUE TO HIGH BMI5.
Compared to 1990, the age-standardized2 obesity prevalence more than doubled for women (from 8.8% to 18.5%) and nearly tripled for men (from 4.8% to 14%), while the overall number of adults with obesity more than quadrupled from 194 million to 878 million.
Should current growth trends continue, obesity prevalence among adults over the age of 20 years is projected to rise to 17% of men and 22% of women by 20303. There is concern potential that almost 2 in 3 adults over the age of 25 years could be affected by overweight or obesity by 20504.
COUNTRIES HAD VARYING LEVELS OF OBESITY PREVALENCE IN 2022. PREVALENCE WAS HIGHEST AMONG WOMEN IN TONGA. AMERICAN SAMOA, AND SAMOA (75–81%) AND AMONG MEN IN AMERICAN SAMOA, NAURU AND TOKELAU (67–70%).
It was also high in many other Pacific and Caribbean Island nations, such as the Bahamas and Saint Kitts and Nevis (around 38% for men and around 55% for women) and countries in the Middle East and North Africa region, such as Qatar and Kuwait (39–41% for men) and Egypt and Qatar (53–59% for women). Obesity prevalence was lowest among women in Vietnam, Timor-Leste, and Japan (2–4%) and among men in Ethiopia, Timor-Leste and Rwanda (1–2%). Prevalence was also low (<5%) in other Asian and East African countries.
Obesity increased in nearly every country from 1990 to 2022, with the largest increases observed in the Bahamas for women (from 22.8% to 55.8%) and Romania for men (from 6.7% to 38.3%). Over this period, a decrease in obesity prevalence was only seen among women in Spain (by 4.6 percentage points), France, Moldova and Lithuania (all by 1–2 percentage points).
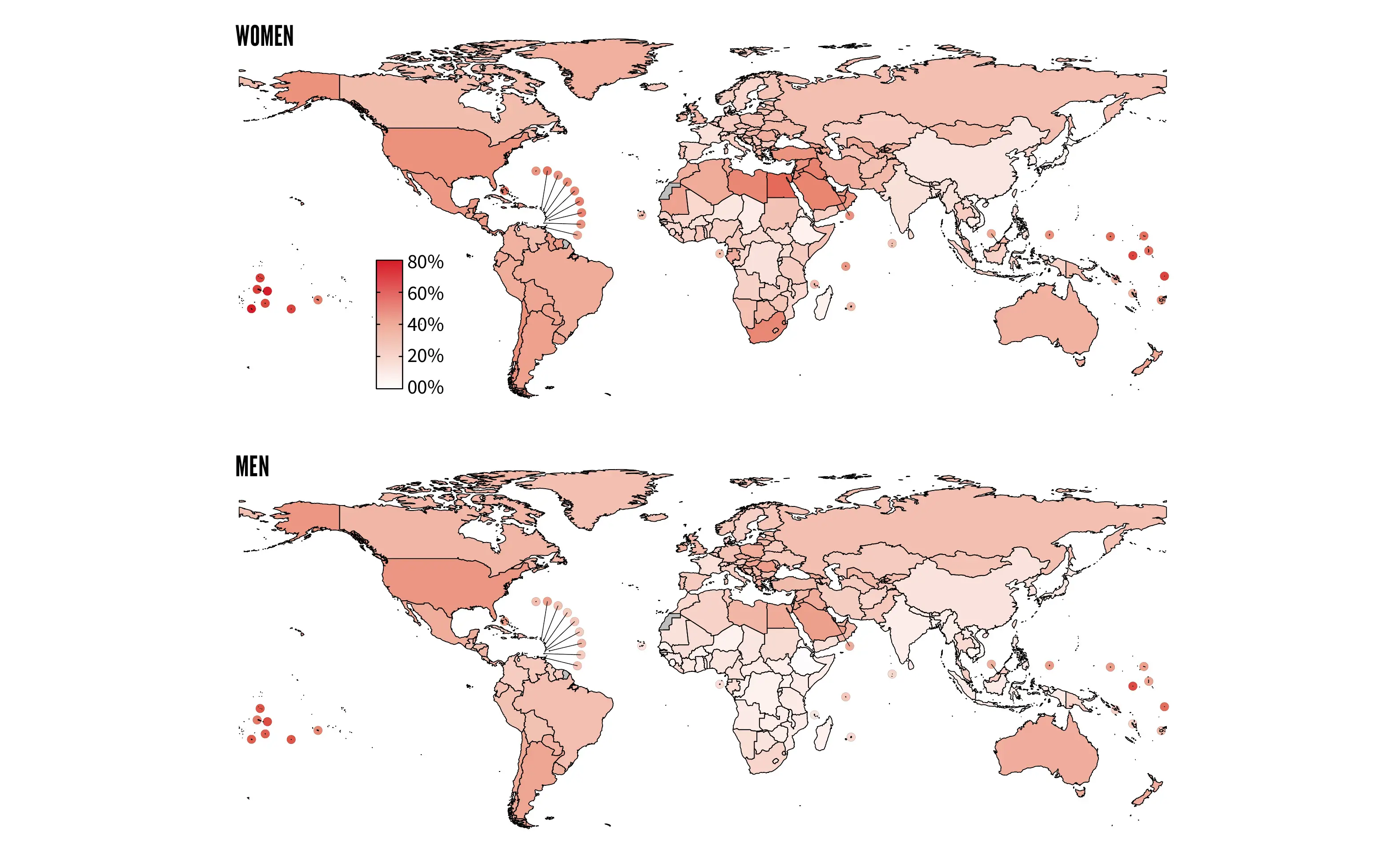
FIGURE 2 - AGE-STANDARDIZED PREVALENCE OF OBESITY IN 2022.
SOURCE: NCD Risk Factor Collaboration.
SOURCE: NCD Risk Factor Collaboration.
The economic impact of obesity
In 2019, the global economic impact of obesity was estimated to be equivalent to 2.2% of global Gross Domestic Product (GDP), or just under US$2 trillion annually69. This figure includes the costs associated with obesity-related healthcare needs, productivity losses and a reduction in human capital from premature death.
If current trends in obesity levels continue, analysts project that the economic impacts will rise to over 3% of GDP per year globally by 2060. This would break down to 2% of GDP in the WHO African Region, over 4% in the WHO Region of the Americas, and over 5% in the WHO Eastern Mediterranean Region. The biggest increases in the economic impact of obesity will be concentrated in LMICs, with significant implications for health systems. Additionally, the impact is projected to triple in high income countries and increase twenty-three-fold in upper middle-income countries.
If coordinated and evidence-based action can reduce obesity and overweight prevalence to 2019 levels, it will translate into savings of US$2.2 trillion in costs every year between 2020 and 2060 globally.
5. GLOBAL CVD MORTALITY ATTRIBUTABLE TO HIGH BMI

OVER THE LAST THREE DECADES, THE NUMBER OF ANNUAL CVD DEATHS GLOBALLY ATTRIBUTABLE TO HIGH BMI (AT LEAST 25 KG/M2 OR OVER) MORE THAN DOUBLED, REACHING 1.9 MILLION IN 2021—MORE THAN HALF OF THE TOTAL 3.7 MILLION DEATHS FROM HIGH BMI AND 9.8% OF TOTAL CVD DEATHS.
READ MORE
Globally, age-standardized CVD-mortality rate attributable to high BMI was 22.8 deaths per 100,000 people in 2021, moderately lower than in 1990 due to the decline in overall CVD mortality.
Regionally, age-standardized CVD mortality rate attributable to high BMI is now highest in middle-income countries and lowest in high-income countries (see Online Appendix Table 1). The age-standardized CVD mortality rate attributable to high BMI ranged from 14.4 deaths per 100,000 people in high-income regions to 67.5 deaths per 100,000 people in North Africa and the Middle East. In 2021, there were an estimated 300,000 more CVD deaths globally attributable to high BMI among women compared with men.
High BMI is the eighth most important risk factor for deaths from CVD globally (Table 1). Since 1990, its risk ranking increased compared to other CVD mortality risk factors—high BMI ranked higher in 2021 compared to 1990 in all but two regions (South Asia, and Southeast Asia, East Asia, and Oceania) where the rankings remained the same.
At the national level, high BMI is the third most important risk factor for CVD mortality in 14 countries, including the Cook Islands, Gabon, and Dominica, while it ranked fourth in an additional 44 countries.
AGE-STANDARDIZED GLOBAL AND REGIONAL CVD MORTALITY ATTRIBUTABLE TO HIGH BMI AND RANKING AMONG ALL RISK FACTORS, FOR BOTH SEXES COMBINED.
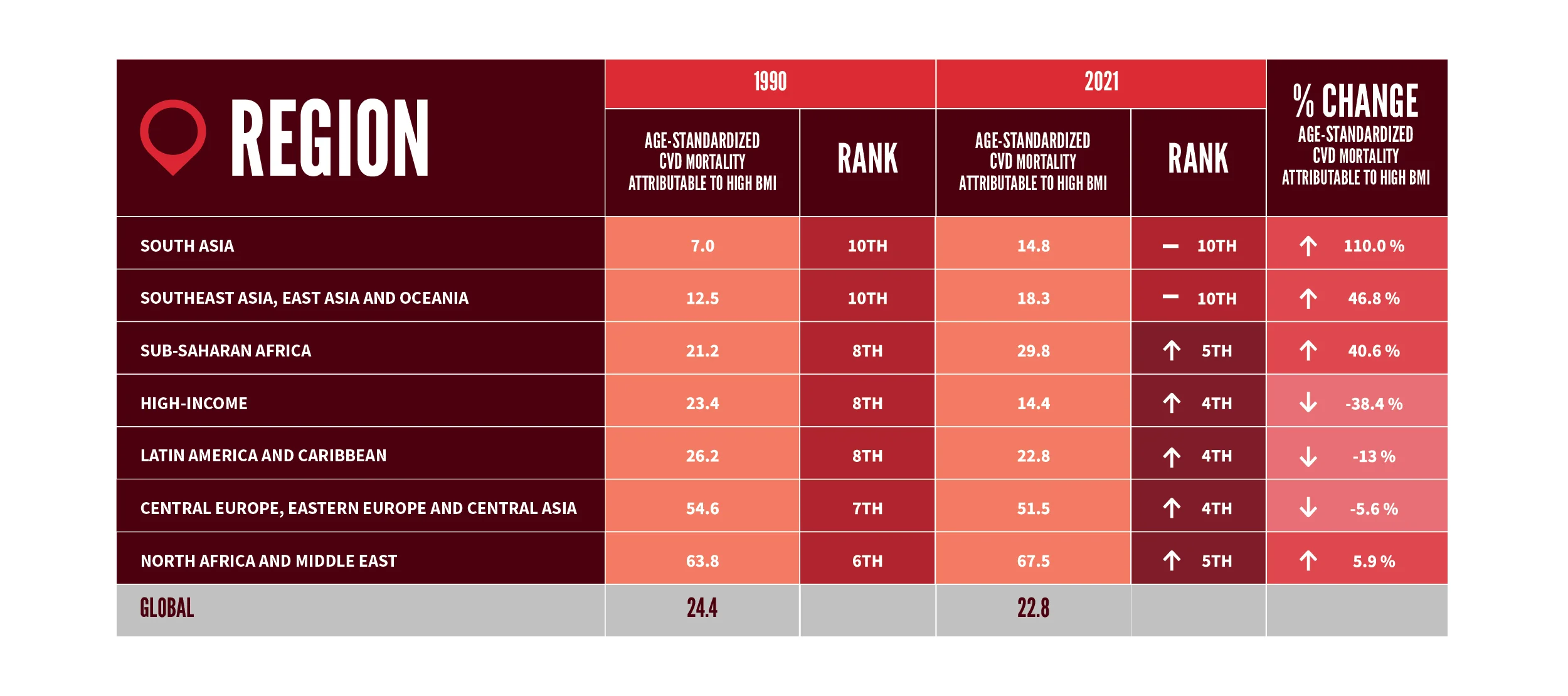
TABLE 1 - SOURCE: INSTITUTE FOR HEALTH METRICS AND EVALUATION.
NOTE: Regional classification based on the Global Burden of Disease classification level; The 12 level 2 risk factors are (in the order of contribution to global CVD mortality in 2021): high systolic blood pressure, dietary risks, air pollution, high LDL cholesterol, tobacco, kidney dysfunction, high fasting plasma glucose, high BMI, non-optimal temperature, other environmental risks, high alcohol use, low physical activity.
NOTE: Regional classification based on the Global Burden of Disease classification level; The 12 level 2 risk factors are (in the order of contribution to global CVD mortality in 2021): high systolic blood pressure, dietary risks, air pollution, high LDL cholesterol, tobacco, kidney dysfunction, high fasting plasma glucose, high BMI, non-optimal temperature, other environmental risks, high alcohol use, low physical activity.
6. DETERMINANTS OF OBESITY AND CVD

Image credit: © World Obesity
OBESITY IS THE RESULT OF MULTIPLE, INTERRELATED FACTORS, INCLUDING SOCIAL, PSYCHOLOGICAL, BIOLOGICAL, ECONOMIC, AND ENVIRONMENTAL THAT CONTRIBUTE TO THE DEVELOPMENT AND PERSISTENCE OF OBESITY AND INCREASED RISK FOR CVDs21.
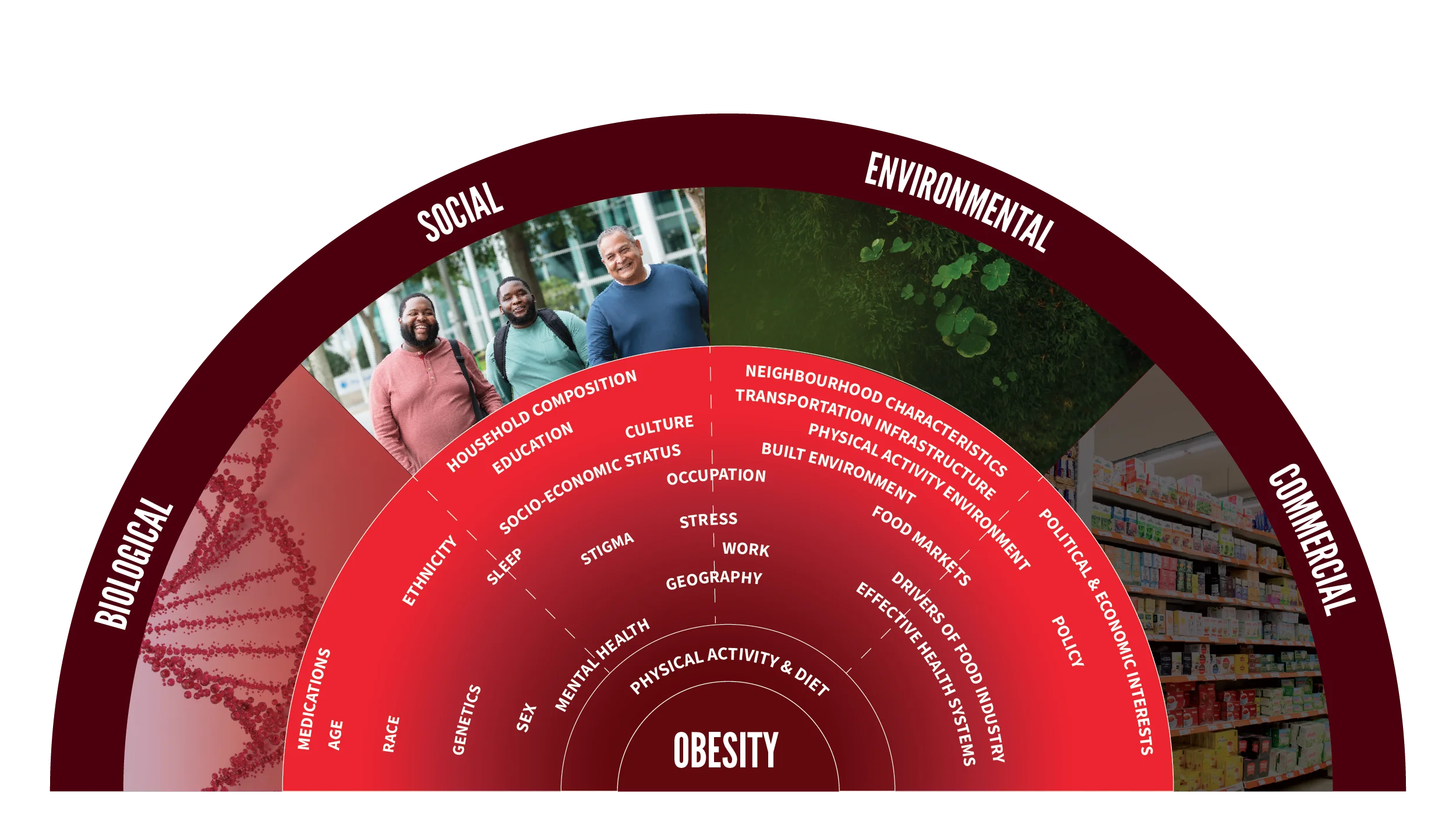
FIGURE 3: DETERMINANTS OF OBESITY AND CVDs.
OBESITY AND STIGMA
People living with overweight or obesity regularly face social stigma, which refers to an “individual's social devaluation and denigration due to their excess body weight, leading to negative attitudes, stereotypes, prejudice, and discrimination.”
READ MORE
People living with obesity can be perceived as lazy, gluttonous, and lacking in self-discipline, with stigmatization manifesting as harmful language or negative portrayals in popular culture and/or media32. This can have long lasting psychological and physical consequences for victims31. Children and young adults are especially vulnerable to bullying and discrimination based on their weight, and obesity is now the leading cause of such bullying in schools, affecting children's education and their mental health36–39.
Within healthcare settings, studies have found some health professionals to hold negative biases about obesity and to spend less time with these patients, viewing them as non-compliant to health advice34,35. This can deter people with obesity from seeking medical care, including prevention and screening, and thereby compromise their overall healthcare.
Long-standing weight stigma and discrimination has hindered efforts to tackle obesity and thus contributed to the rise of CVDs. It is therefore urgent to address weight-based stigma and foster an inclusive society that ensures equity in protection, health, rights, and dignity of individuals, regardless of their body size.
SEX

Image credit: © World Obesity
Obesity prevalence is significantly associated with sex. Women have a higher obesity prevalence than men, and resultantly there is a stronger association between obesity and CVD for women than men22.
READ MORE
Globally the age-standardized prevalence of obesity in 2022 was higher in women than in men by 4.5 percentage points, a figure that has remained largely stable since 1990. Regionally, the obesity disparity between women and men was largest in Central Asia, the Middle East and North Africa, where 40% of women live with obesity compared with 25% of men. Obesity prevalence was also higher in women than men in South Asia, Southeast Asia, Latin America and the Caribbean, Oceania and sub-Saharan Africa. In Central and Eastern Europe, the high-income Western Region and East Asia and the Pacific, obesity prevalence was similar between women and men.
In 2022, women had higher prevalence of obesity than men in over three quarters of countries worldwide (Figure 4), with the difference exceeding 30 percentage points in South Africa, Jamaica, Saint Vincent, and the Grenadines. From 1990 to 2022, the female-male gap in obesity grew larger in most countries in sub-Saharan Africa, Latin America and the Caribbean, Southeast Asia, and in some countries in Central Asia, the Middle East and North Africa. In contrast, the female-male gap in obesity shrank in all countries in Central and Eastern Europe, East Asia, the Pacific, and most high-income western countries. Males have a higher obesity prevalence in 39 countries worldwide.
Socio-cultural, economic, and biological factors all contribute to sex-based differences in obesity.
The association between obesity and CVD differs for men and women. For example, larger waist circumference and waist-to-hip ratio is linked to a greater excess risk of myocardial infarction in women than in men26 and similarly, higher BMI is associated with higher risk of Type 2 diabetes in women than in men27.
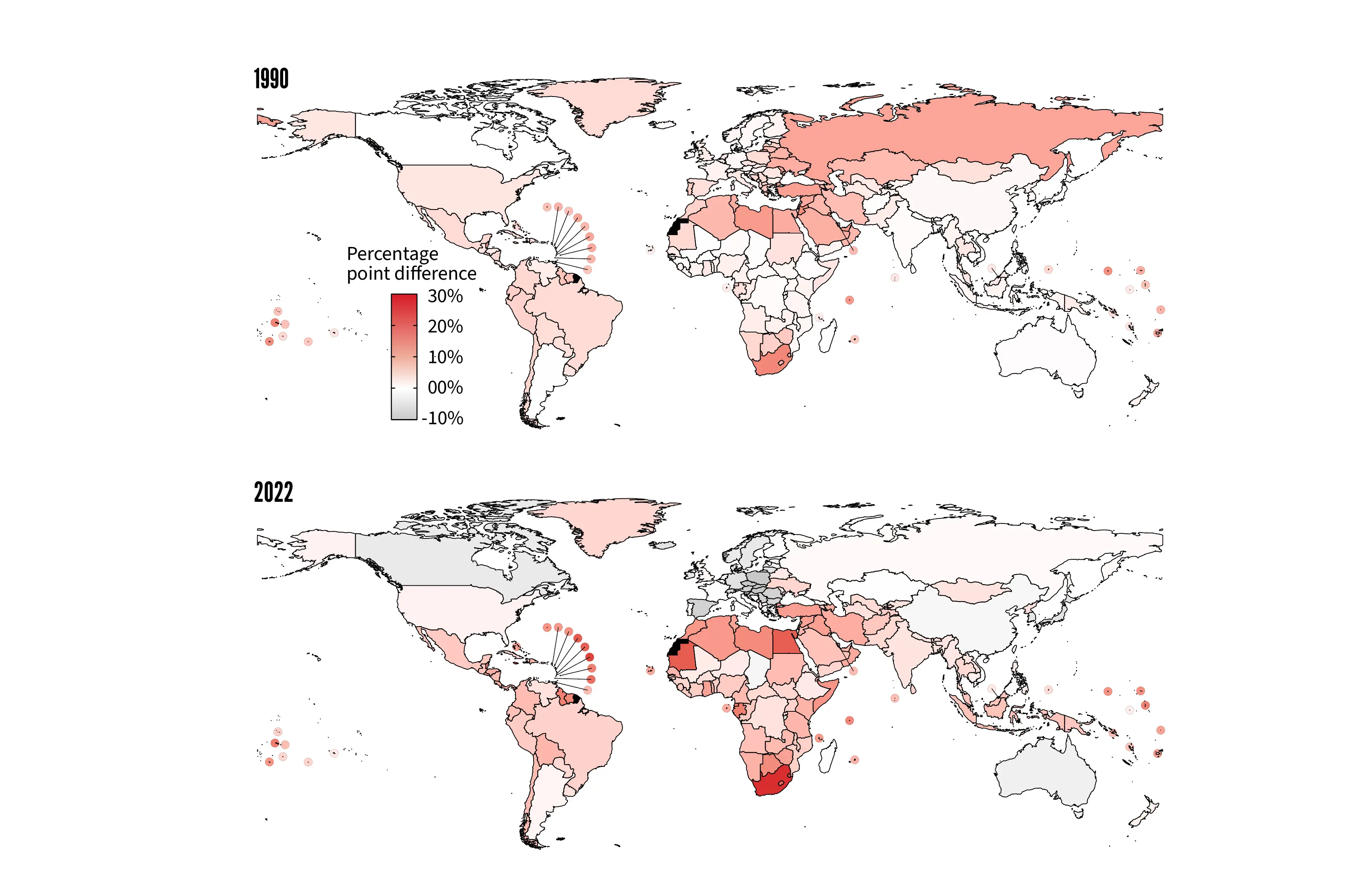
FIGURE 4: ABSOLUTE DIFFERENCE IN THE AGE-STANDARDIZED PREVALENCE OF OBESITY BETWEEN WOMEN AND MEN IN 1990 AND 2022. A POSITIVE DIFFERENCE INDICATES THE PREVALENCE IS HIGHER AMONG WOMEN; A NEGATIVE DIFFERENCE INDICATES THE PREVALENCE IS HIGHER AMONG MEN.
SOURCE: NCD Risk Factor Collaboration.
SOURCE: NCD Risk Factor Collaboration.
FOR WOMEN, 10.8% OF CVD DEATHS ARE ATTRIBUTED TO HIGH-BMI COMPARED TO 8.9% FOR MEN. A SIMILAR PATTERN EXISTS FOR CVD (DALYs), WITH 11.6% FOR WOMEN COMPARED TO 9.8% FOR MEN. GLOBALLY, BMI WAS THE FIFTH HIGHEST CONTRIBUTOR TO CVD DALYs FOR WOMEN, COMPARED TO BEING THE SEVENTH BIGGEST CONTRIBUTOR FOR MEN.
SOCIO-ECONOMIC STATUS

SOCIO-ECONOMIC STATUS (SES) VARIABLES, SUCH AS EDUCATION, INCOME LEVELS AND OCCUPATION, ARE IMPORTANT DETERMINANTS OF OBESITY.
While there are some similarities across countries and regions in the relationship between SES variables and obesity, there are also key differences. For example, in higher-income countries the prevalence of obesity is higher among people with lower levels of education, whereas in LMIC the prevalence of obesity is higher among people with higher levels of education (Figure 5).
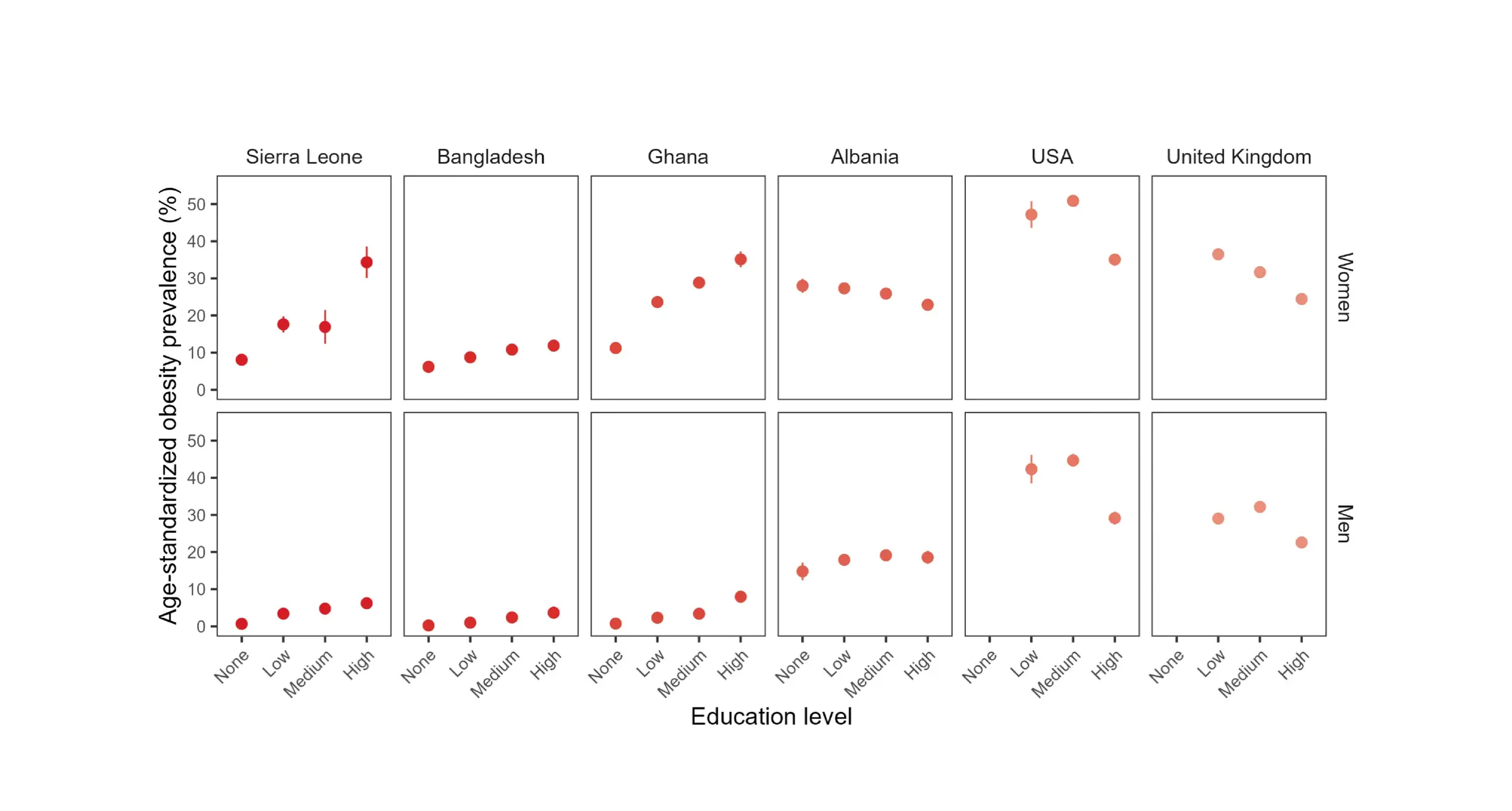
FIGURE 5: AGE-STANDARDIZED PREVALENCE OF OBESITY BY EDUCATION LEVEL IN ADULTS AGED OVER 25 YEARS IN SELECT COUNTRIES.
NOTE: Country income groupings for this figure are as follows - Low-income: Sierra Leone; Lower-middle-income: Bangladesh and Ghana; Upper-middle-income: Albania; High-income: USA and the United Kingdom.
DATA SOURCES: All data are based on publicly available nationally representative health examination surveys, including - Sierra Leone, DHS 2019; Bangladesh, DHS 2022; Ghana, DHS 2022; Albania, DHS 2017–2018; United Kingdom, Health Survey for England 2017–2019, USA NHANES, 2021–2023.
NOTE: Country income groupings for this figure are as follows - Low-income: Sierra Leone; Lower-middle-income: Bangladesh and Ghana; Upper-middle-income: Albania; High-income: USA and the United Kingdom.
DATA SOURCES: All data are based on publicly available nationally representative health examination surveys, including - Sierra Leone, DHS 2019; Bangladesh, DHS 2022; Ghana, DHS 2022; Albania, DHS 2017–2018; United Kingdom, Health Survey for England 2017–2019, USA NHANES, 2021–2023.
ENVIRONMENTAL

PEOPLE’S LIVING ENVIRONMENT PLAYS A MAJOR ROLE IN SHAPING INDIVIDUAL AND POPULATION HEALTH, INCLUDING IN THE DEVELOPMENT OF OBESITY AND CVD.
READ MORE
The term “obesogenic environment” is often used to refer to the role of physical, cultural, social, and economic factors that promote the development of obesity.
It includes structural factors that facilitate the availability and access to safe and easy physical mobility, including infrastructure for walking, running or cycling, and the access and availability of local, sustainable and safe food at locally affordable prices.
In recent years, new concepts have emerged related to people’s food environment, such as food deserts, wherein people, especially those in densely populated urban environments, have limited access to healthy and affordable food. The problems around the food environment are especially stark in LMICs, where the persistence of different forms of undernutrition accompanied by the increase in diet-related NCD risk factors, such as overweight and obesity, have led to the “double burden of malnutrition”.
An increasing number of jobs that require more desk time than physical activity contribute to the development of obesity, too.
THE PSYCHOLOGICAL TOLL OF OBESITY

THE LINK BETWEEN OBESITY AND PSYCHOLOGICAL DISTRESS AND/OR STRESS IS COMPLEX AND MULTI-DIRECTIONAL. STUDIES SHOW A SIGNIFICANT LINK BETWEEN OBESITY AND INCREASED LEVELS OF PSYCHOLOGICAL DISTRESS, SUCH AS DEPRESSION, ANXIETY, EATING DISORDERS AND HOSTILITY, INCLUDING AMONG CHILDREN AND ADOLESCENTS49. THE INTERCONNECTED MECHANISMS LINKING OBESITY AND STRESS ARE A FUNCTION OF COGNITIVE, BEHAVIOURAL AND PHYSIOLOGICAL FACTORS49.
READ MORE
Socio-psychological risk factors, such as stress, are among the determinants of obesity and several social determinants—including financial difficulties, personal conflicts, low self-esteem, and acceptance by peer or social groups—which play a role in the development of chronic stress for people with obesity51,52.
Structured behavioural and lifestyle interventions—especially those involving physical activity and diet—can improve both physical and psychological health in children and adults, even if weight loss is minimal. Mental health considerations should be embedded in weight loss messaging and intervention programmes to address the full scope of obesity’s impact.
URBAN VS RURAL SETTINGS

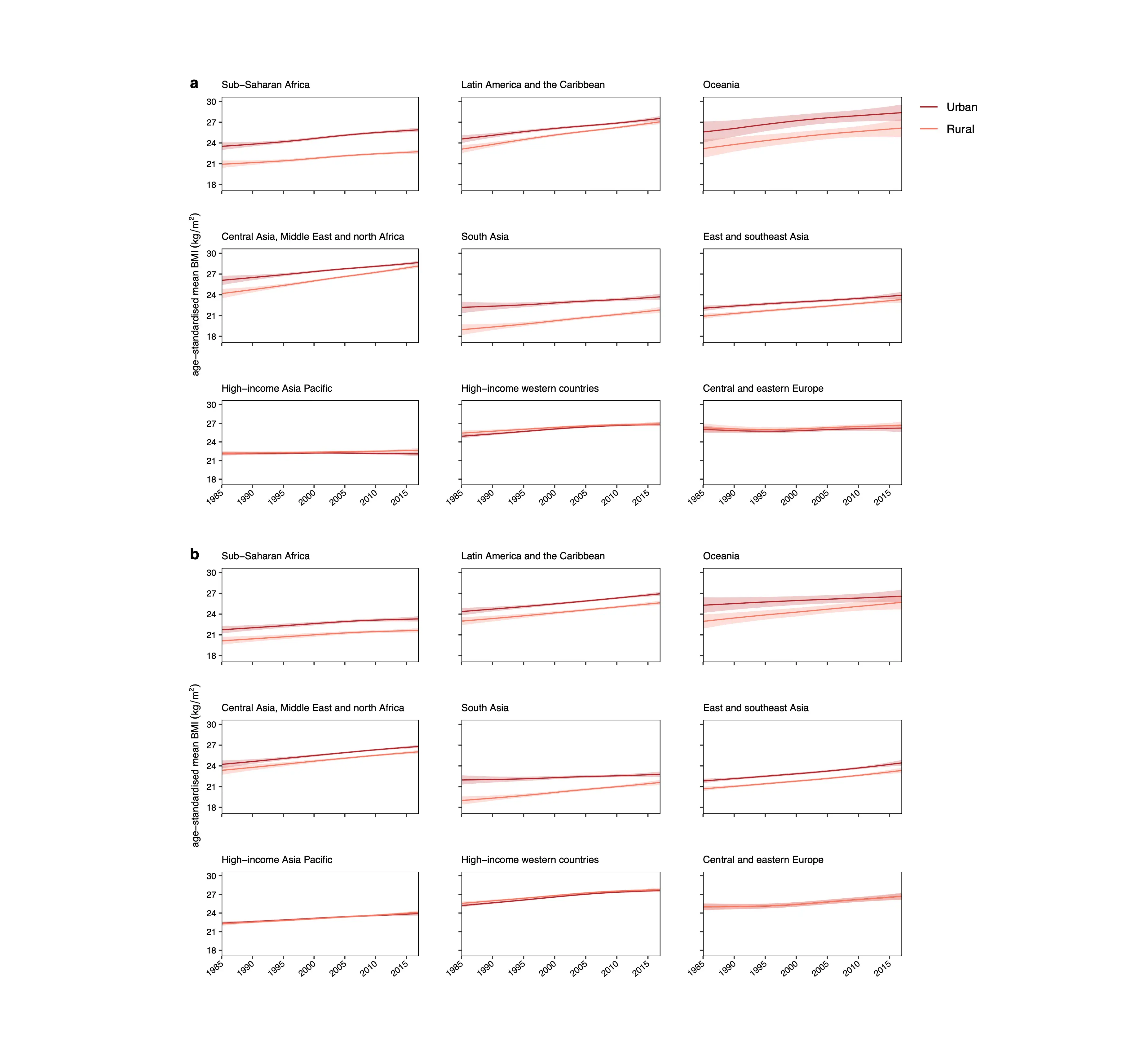
THE PICTURE ON HOW URBAN AND RURAL SETTINGS CONTRIBUTE TO OBESITY AND CVD IS NUANCED. URBANISATION HAS OFTEN BEEN ASSOCIATED WITH INCREASED CVD MORTALITY AND OBESITY PREVALENCE, YET RECENT EVIDENCE SHOWS HOW THE GLOBAL RISE IN AGE-STANDARDIZED MEAN BMI FROM 1985 TO 2017 WAS IN LARGE PART DUE TO THE RISE IN BMI IN RURAL POPULATIONS (FIGURE 6).
READ MORE
While in many LMICs the age-standardized mean BMI of urban residents remains higher than that of their rural counterparts, over the last four decades the faster rise in rural areas has resulted in a rural-to-urban convergence of BMI. For example, in 1985 urban residents in South Asia had higher mean BMI than their rural counterparts (by 3.2 and 3.0 kg/m2 for women and men, respectively), but by 2017, the urban-rural BMI gap had decreased to 1.9 and 1.2 kg/m2 in women and men respectively. This trend was seen during the same period in women in Latin America and the Caribbean, East and Southeast Asia, Central Asia, the Middle East, and North Africa and men in Oceania.
In contrast, women in sub-Saharan Africa saw diverging BMI trends in urban and rural areas with the urban-rural gap widening from 2.6 kg/m2 in 1985 to 3.2 kg/m2 in 2017. Some countries in subSaharan Africa (e.g., Niger and Burkina Faso) had larger urban-rural gaps in BMI than any other country in the world, in part because urbanization has preceded major economic growth in sub-Saharan Africa55.
In high-income and industrialized countries, urban-rural disparities in BMI were less pronounced, with persistently higher BMI in rural areas since 1985 reflecting rural economic and social disadvantage58–60.
COMMERCIAL

COMMERCIAL DETERMINANTS ARE THE WAY IN WHICH COMMERCIAL PRODUCTS, SERVICES AND ACTIVITIES IMPACT PUBLIC HEALTH, DIRECTLY OR INDIRECTLY.
READ MORE
For NCDs, including obesity, this is usually seen in the form of business marketing strategies, labelling, lobbying and other tools to increase consumption of products to increase profits.
Commercial practices contribute significantly to the global burden of NCDs such as obesity and CVD, with 44% of global NCD deaths linked to commercial products and commercial practices61. Commercial practices in the food industry are particularly detrimental to obesity and CVD prevalence. Practices have led environments flooded with unhealthy food that is cheap, accessible, ultra-processed and convenient, yet bad for the population’s health.
BIOLOGICAL

Image credit: © World Obesity
GENETICS CAN PLAY A FUNDAMENTAL ROLE IN DETERMINING AN INDIVIDUAL’S RISK FOR OBESITY. MONOGENIC OBESITY, FOR EXAMPLE, IS CAUSED BY MUTATIONS IN A SINGLE GENE, AND CERTAIN SYNDROMES ARE ASSOCIATED WITH GENETIC ALTERATIONS THAT LEAD TO OBESITY, SUCH AS PRADER-WILLI SYNDROME, BARDET-BIEDL SYNDROME, AND ALSTRÖM SYNDROME. MUTATIONS IN THE LEP (LEPTIN) GENE OR THE LEPR GENE (WHICH ENCODES THE LEPTIN RECEPTOR) CAN DIRECTLY AFFECT APPETITE REGULATION AND FAT STORAGE, LEADING TO SEVERE OBESITY THAT DOES NOT RESPOND TO LEPTIN REPLACEMENT THERAPY63.
READ MORE
Individuals with a genetic predisposition to obesity are more susceptible to adverse environmental factors such as diet, stress, physical activity levels, and exposure to chemicals, all of which can influence epigenetic modifications.
Another important biological determinant of obesity is the composition of the gut microbiota, which plays a key role in digestion, energy extraction, and metabolism. The gut microbiota contributes to energy balance by regulating the production of short-chain fatty acids (SCFAs), which influence energy storage and fat accumulation. Alterations in the microbiota composition, known as gut dysbiosis, are associated with metabolic disorders, including obesity.
7. OBESITY DIAGNOSIS AND CLINICAL MANAGEMENT

Image credit: © World Obesity
Modest weight reductions of 5–10% can lead to substantial improvements in cardiovascular risk factors, such as hypertension, dyslipidaemia, and insulin resistance, while greater weight loss is associated with more pronounced benefits, including reduced incidence of myocardial infarction and stroke.
While patients engaged in weight loss programmes have achieved >5% weight loss, maintenance of this weight loss in the long-term can be challenging for multifactorial reasons.

FIGURE 7: CARDIOVASCULAR BENEFITS OF WEIGHT LOSS
SOURCE: 78
SOURCE: 78
READ MORE
The prevention of obesity and obesity-related CVD in adulthood must ideally begin during and even before childhood. This includes addressing risk factors for childhood obesity such as maternal obesity, maternal diabetes, large-for-gestational age, or breastfeeding for less than six months, among others70. Early detection and screening of childhood obesity should include age-specific and sex-adjusted BMI, assessment of physical activity, and nutritional education in school programmes. All adults should be screened by measurement of BMI, waist-to-hip ratio, waist circumference, impaired fasting glucose/ prediabetes/diabetes, and shortness of breath unrelated to other conditions.
CLINICAL MANAGEMENT
Clinicians play a pivotal role in addressing obesity to prevent and treat CVD and should assess patientsʼ weight status and help implement individualized, evidence-based interventions to promote weight loss and mitigate CVD risk, including through referral to specialist clinicians. Comprehensive and long-term obesity management involves a multidisciplinary approach that can rely on intensive lifestyle management and the establishment of a continuum of care with a primary care physician, including, but not limited to:
Behavioural interventions
De-stigmatisation of obesity
Nutritional guidance to determine individualized dietary programmes that are pragmatic and realistic

Physical activity promotion

Pharmacotherapy or surgery
In adults with increasingly excess weight, minimally invasive surgery can be an effective long-term treatment, with about 90% of patients achieving at least 15–40% weight loss and the improvement in obesity-related conditions.
MEDICATIONS FOR TREATING OBESITY
Medications for obesity, when used in conjunction with lifestyle interventions, can be effective in increasing weight loss and, when used appropriately, maintaining it in the long term72. These medications can include stimulants, central nervous system acting agents, and gastrointestinal malabsorption agents.
READ MORE
Recently, more novel treatments known as glucagon-like peptide-1 receptor agonists (GLP-1RAs) and their analogues (originally developed to treat diabetes) are used in treatment plans. GLP-1RAs are naturally occurring incretins released by the intestine after a meal that work by delaying gastric emptying, thus acting peripherally to decrease hunger, and increase insulin sensitivity, among other effects. GLP-1RAs and their analogues are shown to treat cardiometabolic disease by improving outcomes across several areas—including weight loss, waist circumference, glucose control, dyslipidaemia, diabetes, blood pressure, and inflammation—decreasing major adverse cardiovascular events for secondary prevention73, and improving symptoms in patients with heart failure with preserved ejection fraction (HFpEF)74,75. There is growing evidence that these classes of medications benefit all organ systems through decreasing inflammation and increasing weight loss76. Tirzepatide, a dual GLP-1RA/GIP analogue, is the first medication that has been FDA approved to treat obstructive sleep apnea74.
GLP-1RAs have transformed the medical management of obesity as earlier medications provided modest weight loss (<5-10%) and had challenging side effects for patients72.
CHALLENGES IN CARDIOVASCULAR EVALUATION AND MANAGEMENT OF PATIENTS WITH OBESITY
Obesity can complicate cardiovascular diagnosis, management, and treatment.
This underscores the importance of a multidisciplinary approach for managing obesity in cardiovascular disease, and integrating medical, lifestyle, pharmacologic, and/or surgical strategies tailored to each patient’s needs. Given the high prevalence of obesity in populations experiencing cardiovascular problems, future clinical guidelines should incorporate obesity-specific recommendations to improve patient outcomes77.
1
DIAGNOSIS
The presence of excess fat (adipose tissue) can result in:
- Less accurate or distorted electrocardiograms.
- Poor acoustic windows or limited penetration with transthoracic echocardiograms.
- Reduced accuracy of stress tests.
- Reduced accuracy for imaging (single-photon emission computerized tomography (SPECT), cardiovascular magnetic resonance imaging (CMR), and computed tomography coronary angiography (CTCA).
2
TREATMENT

PHARMACOLOGICAL
Obesity significantly alters drug pharmacokinetics and pharmacodynamics, affecting how medications are absorbed, distributed, metabolized, and eliminated. For example:
- Lipophilic drugs (drugs that are fat-soluble, allowing them to cross cell membranes to enter cells or fatty tissue e.g., atorvastatin, timolol) may have an increased volume of distribution.
- Renal and hepatic clearance of drugs can be unpredictable, requiring careful dose adjustments to avoid under- or over-dosing.
- Anticoagulant dosing presents a challenge in obesity, as there is limited evidence to guide appropriate adjustments for direct-acting oral anticoagulants (DOACs). Higher body weight may reduce drug concentrations, increasing the risk of thrombosis, while excessive dosing could raise the likelihood of bleeding, creating a difficult balance in anticoagulation therapy.
Although new medications (e.g., GLP-1RAs) achieve substantial weight loss, their effects on mental health are mixed, necessitating further long-term research.
SURGICAL
- Percutaneous coronary interventions in people with obesity pose technical difficulties, including challenges with vascular access, higher risks of stent thrombosis, and complications related to haemostasis. The radial artery is often preferred for access in patients with obesity, as femoral access is more challenging and associated with higher bleeding risks.
- Cardiac surgery outcomes in people with obesity are associated with higher complication rates, including increased incidence of atrial fibrillation, surgical wound infections, prolonged ventilation, and renal failure.
- People with severe obesity undergoing coronary artery bypass grafting (CABG) have higher long-term cardiovascular mortality, underscoring the need for preoperative risk optimization.
3
MANAGEMENT

- Lifestyle interventions, such as physical activity, can be hindered by physical limitations such as joint pain, obstructive sleep apnoea, and deconditioning, all of which can make regular exercise challenging.
- Dietary modifications can be complicated by conflicting recommendations, making it crucial for clinicians to provide clear, personalized guidance on sustainable weight management strategies. For example, a patient with diabetes, chronic kidney disease and heart disease will get recommendations to consume less carbohydrates, protein and fat, potentially creating confusion and reducing dietary options.
- Cardiac rehabilitation programmes are underutilized for weight management, despite their potential role in improving cardiovascular health. Only a small percentage of rehabilitation programmes include structured weight-loss components, yet long-term lifestyle interventions, particularly group-based approaches, have been shown to improve metabolic and functional outcomes in people with obesity.
- Mood disorders, particularly anxiety and depression, are common in individuals with obesity and cardiovascular disease, leading to poor adherence to treatment and worsening health outcomes.
4
OTHER

In some cases, treatments for CVDs and other health issues can contribute to obesity, usually as a side effect. For example:
- Beta-blockers are associated with metabolic effects that can lead to weight gain, potentially worsening insulin resistance, increasing fatigue, and reducing exercise tolerance. Metoprolol tartrate has been linked to weight gain, while carvedilol may have a more favourable metabolic profile, making drug selection an important consideration.
- Depression is linked to increased cardiovascular risk, and antidepressant therapy may further contribute to weight gain, creating a cycle that requires careful psychological and medical management.
8. Public health interventions to address obesity and CVD

Image credit: © World Obesity
In addition to individual-focused interventions, public health interventions play a vital role in reducing the incidence and impact of obesity and CVD1. These include:
- Community-focused interventions—urban planning, the development of safe spaces for exercise, school-based programmes and enhancing access to nutritious foods— that can establish supportive environments that facilitate healthy behaviours.
- System-level interventions—policies that regulate food marketing and tax sugary drinks, subsidise healthy food options and integrate health promotion into urban planning—that can address structural barriers to health. Health-system level interventions to improve access to and quality of care are also important measures to reduce the burden of obesity and CVD79,80.
Any policy to tackle obesity must address health disparities through prioritising underserved populations who face greater barriers to healthy living. This includes ensuring access to healthcare, targeting interventions in low-income communities and tailoring policies to cultural and social contexts.
CITY-LEVEL APPROACHES
A city approach provides a cohesive framework where various interventions across health, urban planning, transportation and education, among others, can create healthier environments81. For example, healthy cities policies focus on designing environments that promote physical activity and access to nutritious food, while urban planning initiatives, such as creating walkable neighbourhoods, expanding cycling infrastructure and increasing green spaces, encourage active transportation and recreational physical activity.
NUTRITION AND FOOD
RELATED INTERVENTIONS
There are several regulatory, tax- and programme-based initiatives that governments can implement to reduce the incidence of obesity and CVD. For example, many governments have successfully imposed tax policies on sugary drinks and unhealthy foods, which discourage consumption while generating public revenue for health promotion84.
BEHAVIOURAL AND EDUCATIONAL INTERVENTIONS
Public health campaigns that aim to change behaviours can include media campaigns to raise awareness about the importance of healthy diets and physical activity88,89, school-based programmes to promote lifelong habits through education on nutrition and fitness, and workplace wellness initiatives to incentivise employees to adopt healthier lifestyles88,90.
POLICY INTEGRATION AND CROSS-SECTOR
Addressing obesity and CVD requires integrating health objectives into policies across sectors such as transportation, urban planning, education and agriculture. Multisectoral collaboration ensures that health considerations are embedded into non-health policies, maximising their impact on population health1,84,85,91.
HEALTH SYSTEM INTERVENTIONS
Interventions to support health systems to provide affordable, available and sustainable health services to prevent, treat and manage obesity are essential. The 2023 “WHO Health service delivery framework for prevention and management of obesity” provides countries with guidance on how to integrate and organise obesity prevention and management services throughout the health system, with a focus on applying a primary, chronic and integrated care approach.
Examples of policies and interventions to address obesity and cardiovascular disease Policy & intervention map
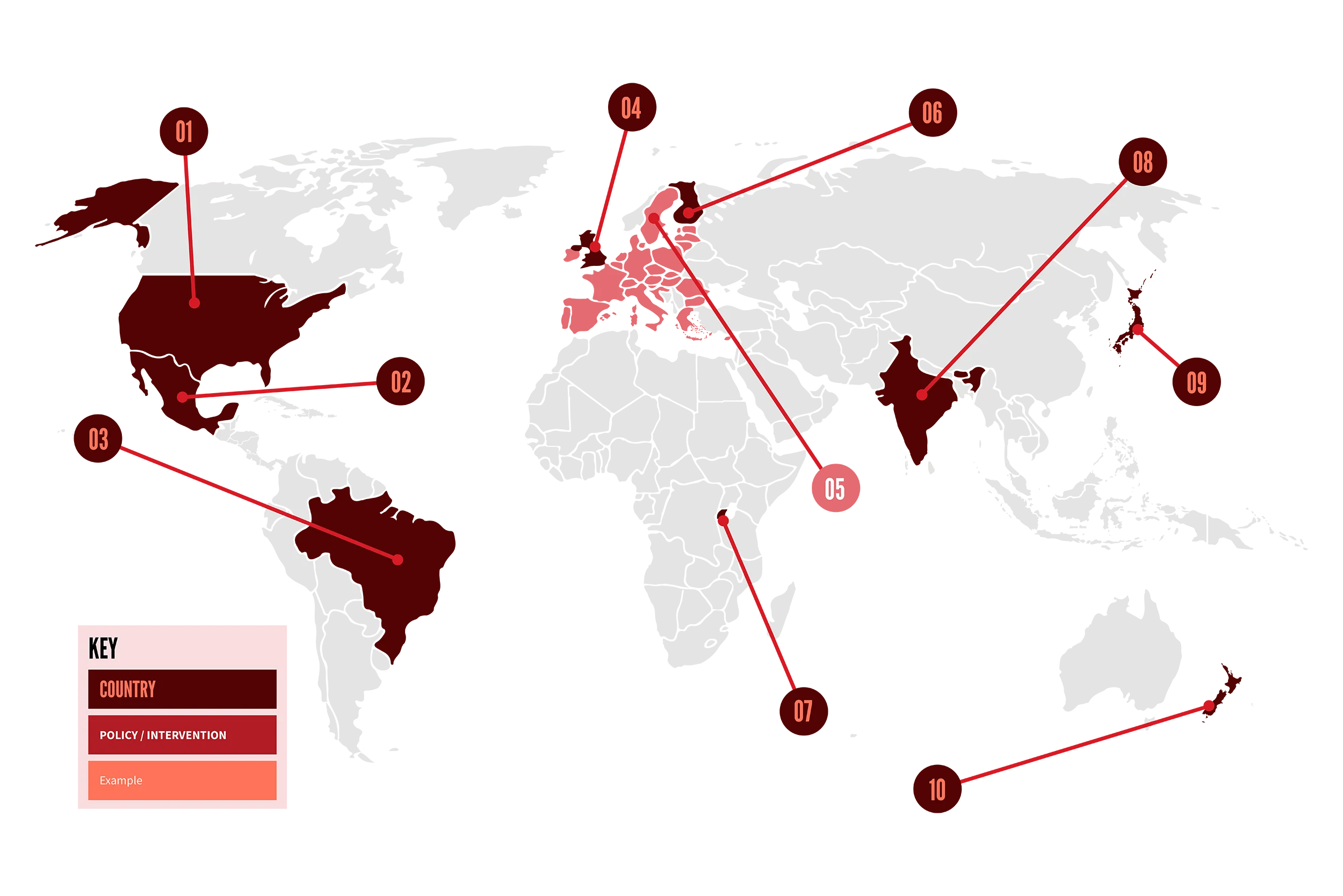
01 - UNITED STATES
ELIMINATING FOOD DESERTS
The Healthy Food Financing Initiative (HFFI) in the United States provides funding to eligible organizations that are planning to develop a food retail outlet or food supply chain that will improve access to staple and perishable foods in underserved areas97.
02 - MEXICO
TAXATION ON UNHEALTHY FOODS AND SUGARY DRINKS
In 2014, Mexico introduced a sugar-sweetened beverage tax of 1 peso per liter, equivalent to about 10% of the price of sugary drinks95.
03 - BRAZIL
FRONT-OF-PACK LABELLING
In 2020, a new regulation was approved in Brazil stating that the nutritional labelling must be placed on the front panel of packaged foods using simple and clear icons to emphasize high contents of saturated fat, added sugar and sodium96.
04 - UK
ZONING REGULATIONS
In 2015, the Gateshead council in the UK implemented a comprehensive restriction preventing the opening of any new fast food establishments with the aim of reducing childhood obesity to less than 10% by 2025 from 22.6% in 2015.(*No new fast-food outlets allowed! Evaluating the effect of planning policy on the local food environment in the North East of England)94.
05 - EUROPEAN UNION
PROMOTE SUSTAINABLE FOOD SYSTEMS
The European Union (EU) ‘Farm to Fork’ strategy, a part of the European Green Deal, aims to promote sustainable food systems, while ensuring availability of sufficient nutritious, safe and sustainable food within EU countries103.
06 - FINLAND
SCHOOL MEAL PROGRAMMES
Finland school meal programme, providing free balanced and healthy school meals to each child and young person attending pre-primary, primary, lower secondary and upper secondary education98.
07 - RWANDA
REDUCING HEALTH DISPARITIES
The Rwandan Community Based Health Insurance promotes access to medical care at affordable cost for underserved communities. Through this system, individuals are able to receive primary medical care, including services for the prevention and management of CVD and obesity, from health centres or healthposts across the country106.
08 - INDIA
PUBLIC HEALTH CAMPAIGNS
The “Eat Right India” campaign launched in 2018 by the Food Safety and Standards Authority of India (FSSAI), designed to promote healthy eating and raise awareness about the importance of balanced diets to prevent obesity. It uses mass media, including TV, radio and digital platforms, to spread messages on nutrition, food safety and the dangers of overeating99.
09 - JAPAN
SCHOOL-BASED PROGRAMMES
In 2005, Japan implemented a nationally mandated food education programme called Shokuiko, teaching students about balanced nutrition, food origins and healthy eating habits. Schools provide nutritionally balanced meals, and students are actively involved in food preparation and meal planning to instill lifelong healthy eating habits100.
10 - NEW ZEALAND
ADDRESS CHRONIC DISEASES
The Mana Tū project, co-designed with Māori and Pasifika communities to address chronic diseases, such as diabetes and CVD, was implemented in New Zealand from 2017 to 2020. Through the project, communities received support and guidance around different areas closely related to effective disease management, including nutrition. Thanks to this project, the amount of fruit and vegetables consumed by participants increased, alongside a10% average increase in physical activity105.
9. Global initiatives to address obesity and CVD

ROBUST GLOBAL STRATEGIES SUPPORT NATIONAL AND LOCAL EFFORTS TO REDUCE OBESITY AND CVD, AS THEY HELP IN DEFINING SPECIFIC OBJECTIVES AND GOALS FOR ADDRESSING OBESITY AND PROVIDE GUIDANCE ON EFFECTIVE SOLUTIONS TO CURB ITS GROWING PREVALENCE.
1
GLOBAL ACTION PLAN FOR THE PREVENTION AND CONTROL OF NONCOMMUNICABLE DISEASES (2013–2020 EXTENDED UNTIL 2030)
Overview: WHO’s “Global Action Plan” provides a roadmap for countries to develop and implement national strategies to prevent and manage NCDs, including obesity, with the aim of reducing premature deaths from NCDs by 25% by 2025. The Plan includes specific targets and key actions across various areas, with a focus on reducing risk factors such as unhealthy diets, physical inactivity, tobacco use, and harmful use of alcohol. The monitoring framework developed to track progress in reducing the burden of NCDs includes a set of indicators linked to 9 voluntary targets.
2
ACCELERATION PLAN TO STOP OBESITY (2022)
Overview: WHO’s “Acceleration Plan to Stop Obesity” is designed to stimulate and support multisectoral actions at the national level based on evidence-informed policies. It takes a systematic approach to addressing obesity through helping countries to navigate the complexities of implementation challenges and delivering results. This includes through a consolidated set of policy recommendations shown to be effective, affordable, adaptable, and scalable to deliver positive outcomes for people with obesity.
Notable policies: Among the recommendations are policies to support:
Protection of individuals from the harmful advertising of unhealthy foods.
Taxes on unhealthy foods and reformulation of food products.
Promotion of physical activity and nutritional education in schools.
Greater integration of obesity prevention and treatment into primary healthcare services, especially in LMICs where resources are limited.
3
THE GLOBAL STRATEGY ON DIET, PHYSICAL ACTIVITY AND HEALTH (2024)
Overview: WHO’s “Global Strategy on Diet, Physical Activity and Health” aims to reduce the global burden of NCDs, including CVD and obesity, through improved diet and physical activity. This strategy provides clear objectives and actions to mitigate the risk factors contributing to these diseases.
Objectives: The Global Strategy lists four main objectives:
1
Reduce the risk factors for NCDs that stem from unhealthy diets and physical inactivity by means of essential public health action and health-promoting and disease preventing measures.
2
Increase the overall awareness and understanding of the influences of diet and physical activity on health and of the positive impact of preventive interventions.
3
Encourage the development, strengthening and implementation of global, regional, national and community policies and action plans to improve diets and increase physical activity that are sustainable, comprehensive, and actively engage all sectors, including civil society, the private sector and the media.
4
Monitor scientific data and key influences on diet and physical activity, support research in a broad spectrum of relevant areas, including evaluation of interventions, and strengthen the human resources needed in this domain to enhance and sustain health.
4
THE WHO GLOBAL ACTION PLAN ON PHYSICAL ACTIVITY (2018–2030)
Overview: The Plan responds to global calls for stronger action and coordination to reverse physical inactivity trends, a major contributor to NCDs, and sets out a system-wide, multisectoral framework for promoting physical activity through urban design, education, health systems, transport, sports, and community engagement. It complements the WHO “Global Action Plan on NCDs 2013–2020”.
Goal: 15% relative reduction in the global prevalence of physical inactivity among adults and adolescents by 2030, using 2016 as a baseline.
Objectives: The Plan includes four strategic objectives, supported by 20 evidence-based policy actions including:
1
Create active societies, supported by four policy actions to shift social norms and attitudes towards.
2
Create active environments, supported by five policy actions to build safe and accessible infrastructure.
3
Create active people, supported by six policy actions to expand access to programmes and opportunities.
4
Create active systems, supported by five policy actions to strengthen governance, partnerships, data systems.
5
UNITED NATIONS DECADE OF ACTION ON NUTRITION (2016–2025)
Overview: The UN launched this global initiative to address malnutrition in all its forms, including undernutrition, micronutrient deficiencies, and overnutrition, with a focus on promoting healthy diets to improve public health. It is part of the broader UN strategy to achieve the Sustainable Development Goals.
Main areas: Action during the Nutrition Decade is based on 6 thematic areas:
1
Sustainable, resilient food systems for healthy diets.
2
Aligned health systems providing universal coverage of essential nutrition actions.
3
Social protection and nutrition education.
4
Trade and investment for improved nutrition.
5
Safe and supportive environments for nutrition at all ages.
6
Strengthened governance and accountability for nutrition.
While these actions are not accompanied by specific targets, they serve as useful guidance for governments aiming to implement policies and strategies to improve nutrition, which in turn will have an impact on CVD prevalence and mortality.
6
UPCOMING: WHO TECHNICAL PACKAGE TO STOP OBESITY
On World Obesity Day 2025 (March 4), WHO announced the launch of a new “Technical Package to Stop Obesity” that extends beyond the WHO “Acceleration Plan to Stop Obesity”. As per the announcement, “the technical package provides a practical how-to approach of proven interventions selected by countries according to their own priorities and tailored to a local context”.
10. KEY RECOMMENDATIONS

ALL COUNTRIES AND STAKEHOLDERS MUST URGENTLY WORK TOGETHER TO ACCELERATE EFFORTS TO REDUCE THE MORTALITY AND MORBIDITY BURDEN OF OBESITY AND CVDS THROUGH THE IMPLEMENTATION OF EVIDENCE-INFORMED PUBLIC HEALTH AND CLINICAL INTERVENTIONS.
Public health interventions
1
All countries should implement evidence-based, cost-effective public health measures to address obesity and CVD, and prioritize comprehensive, integrated and equity-focused policies guided by national data on how determinants vary across population groups. Implementation should draw on global frameworks and tools. Priority actions include national obesity roadmaps with defined targets, multisectoral policies addressing the broad scope of obesity determinants, and ensuring greater integration of obesity prevention and treatment into primary healthcare services.
2
Public health campaigns and policies must counteract the stigmatization of obesity, including through the use of person-first language, recognizing that stigma is a hindrance to tackling obesity and CVD. This includes acknowledging the broad determinants of obesity and implementing legislation to address discrimination of people with obesity and overweight. To achieve best results, the design of campaigns and policy initiatives should involve people living with obesity and CVD.
CLINICAL INTERVENTIONS
1
Cardiovascular guidelines should incorporate obesity-specific recommendations to ensure CVD management is adequately adapted for people living with obesity. This includes equipping health professionals with the knowledge, guidance and tools necessary to optimally prevent, manage and treat obesity.
2
Health professional education and health system strengthening initiatives for obesity and CVD should focus on promoting person-centred, integrated care and where possible be responsive to disparities in obesity risk, prevalence and access to care.
3
Governments should increase efforts to expand the availability and affordability of obesity medications, such as GLP-1RAs.
4
Governments should increase efforts to expand the public awareness, availability and accessibility of specialized lifestyle modification programmes, including those targeting children and adolescents.
RECOMMENDATIONS TO IMPROVE RESEARCH AND DATA
Governments, academia, the private sector and others must collaborate to enhance research and data collection efforts to improve the response to obesity and CVD. Required actions include, but are not limited to:
1
Increase investment and enhance collaboration in research to, among other areas, improve recommendations for the optimal management and treatment of obesity in people with CVD.
2
Improve global and regional data collection to better inform global levels and trends of obesity and attributable mortality/morbidity. Existing estimates result from complex statistical models (see Online Appendix), yet there are important gaps in the data that inform these models, particularly in certain geographies where limited data result in high levels of uncertainty in the final estimates.
3
Address limitations in data on the major drivers of obesity. These hinder disease mitigation efforts—particularly due to the lack of harmonized and comparable data on factors such as education, occupation, and income—and our understanding of whether the obesity epidemic is impacting different population subgroups equally and at the same pace.
4
Prioritise dissemination and implementation of research that explores the local socio-economic, cultural, and environmental factors influencing obesity, especially in LMICs.
5
Prioritise research that examines the impact of social determinants of health (e.g., poverty, low educational attainment, housing insecurity, urbanization, food insecurity, access to healthcare) on obesity and cardiometabolic risk.
6
Support training and career development for the next generation of researchers and clinicians with interest in obesity research across the lifespan.
7
Support research to develop and test strategies in the effectiveness of early childhood and school-based obesity prevention programmes, and support the scale-up of such strategies when proven effective in specific settings.
REFERENCES
1. World Health Organization. WHO Acceleration Plan to Stop Obesity. World Health Organization; 2023. https://play.google.com/store/books/details?id=86IOEQAAQBAJ
2. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet. 2024;403(10431):1027-1050. doi:10.1016/S0140-6736(23)02750-2
3. World Obesity Atlas 2025. World Obesity Federation; 2025. https://data.worldobesity.org/publications/world-obesity-atlas-2025-v6.pdf
4. Global, regional, and national prevalence of adult overweight and obesity, 1990–2021, with forecasts to 2050: a forecasting study for the Global Burden of Disease Study 2021. The Lancet. 2025;405(10481):813-838. doi:10.1016/S0140-6736(25)00355-1
5. Institute for Health Metrics and Evaluation (IHME). GBD Compare Data Visualization. 2024. Accessed March 11, 2025. http://vizhub.healthdata.org/gbd-compare
6. de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660-667. doi:10.2471/blt.07.043497
7. Sweatt K, Garvey WT, Martins C. Strengths and limitations of BMI in the diagnosis of obesity: What is the path forward? Curr Obes Rep. 2024;13(3):584-595. doi:10.1007/s13679-024-00580-1
8. Rubino F, Cummings DE, Eckel RH, et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. Published online January 9, 2025. doi:10.1016/S2213-8587(24)00316-4
9. Lopez-Jimenez F, Almahmeed W, Bays H, et al. Obesity and cardiovascular disease: mechanistic insights and management strategies. A joint position paper by the World Heart Federation and World Obesity Federation. Eur J Prev Cardiol. 2022;29(17):2218-2237. doi:10.1093/eurjpc/zwac187
10. Ralston J, Cooper K, Powis J. Obesity, SDGs and ROOTS: a Framework for Impact. Current Obesity Reports. 2021;10(1):54. doi:10.1007/s13679-020-00420-y
11. Di Cesare M, Sorić M, Bovet P, et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Medicine. 2019;17(1):1-20. doi:10.1186/s12916-019-1449-8
12. Brady TM. Obesity-Related Hypertension in Children. Frontiers in pediatrics. 2017;5. doi:10.3389/fped.2017.00197
13. Cook S, Kavey RE. Dyslipidemia and pediatric obesity. Pediatric clinics of North America. 2011;58(6). doi:10.1016/j.pcl.2011.09.003
14. Pulgaron ER, Delamater AM. Obesity and type 2 diabetes in children: epidemiology and treatment. Current diabetes reports. 2014;14(8). doi:10.1007/s11892-014-0508-y
15. Raj M. Obesity and cardiovascular risk in children and adolescents. Indian journal of endocrinology and metabolism. 2012;16(1). doi:10.4103/2230-8210.91176
16. Chung ST, Krenek A, Magge SN. Childhood Obesity and Cardiovascular Disease Risk. Current Atherosclerosis Reports. Published online May 31, 2023:1. doi:10.1007/s11883-023-01111-4
17. How to stop obese children having heart disease in adulthood. Accessed March 28, 2025. https://www.escardio.org/The-ESC/Press-Office/Press-releases/How-to-stop-obese-children-having-heart-disease-in-adulthood
18. EASO Secretariat. Severe obesity in childhood can halve life expectancy, global modelling study finds. EASO. May 14, 2024. Accessed March 28, 2025. https://easo.org/severe-obesity-in-childhood-can-halve-life-expectancy-global-modelling-study-finds/
19. Bleich SN, Vercammen KA, Zatz LY, Frelier JM, Ebbeling CB, Peeters A. Interventions to prevent global childhood overweight and obesity: a systematic review. Lancet Diabetes Endocrinol. 2018;6(4):332-346. doi:10.1016/S2213-8587(17)30358-3
20. Welsh A, Hammad M, Piña IL, Kulinski J. Obesity and cardiovascular health. Eur J Prev Cardiol. 2024;31(8):1026-1035. doi:10.1093/eurjpc/zwae025
21. Powell-Wiley TM, Baumer Y, Baah FO, et al. Social determinants of cardiovascular disease. Circ Res. 2022;130(5):782-799. doi:10.1161/CIRCRESAHA.121.319811
22. Manrique-Acevedo C, Chinnakotla B, Padilla J, Martinez-Lemus LA, Gozal D. Obesity and cardiovascular disease in women. Int J Obes (Lond). 2020;44(6):1210-1226. doi:10.1038/s41366-020-0548-0
23. Jung NM, de Bairros FS, Pattussi MP, Pauli S, Neutzling MB. Gender differences in the prevalence of household food insecurity: a systematic review and meta-analysis. Public Health Nutr. 2017;20(5):902-916. doi:10.1017/S1368980016002925
24. Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6(10):e1077-e1086. doi:10.1016/S2214-109X(18)30357-7
25. Sfm C, Van Cauwenberg J, Maenhout L, Cardon G, Lambert EV, Van Dyck D. Inequality in physical activity, global trends by income inequality and gender in adults. International Journal of Behavioral Nutrition and Physical Activity. 2020;17(1):1-8. doi:10.1186/s12966-020-01039-x
26. Peters SAE, Bots SH, Woodward M. Sex differences in the association between measures of general and central adiposity and the risk of myocardial infarction: Results from the UK Biobank. J Am Heart Assoc. 2018;7(5). doi:10.1161/JAHA.117.008507
27. Censin JC, Peters SAE, Bovijn J, et al. Causal relationships between obesity and the leading causes of death in women and men. PLoS Genet. 2019;15(10):e1008405. doi:10.1371/journal.pgen.1008405
28. Kivimäki M, Smith GD, Juonala M, et al. Socioeconomic position in childhood and adult cardiovascular risk factors, vascular structure, and function: cardiovascular risk in young Finns study. Heart. 2006;92(4):474-480. doi:10.1136/hrt.2005.067108
29. Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87(5):1107-1117. doi:10.1093/ajcn/87.5.1107
30. O’Donoghue G, Kennedy A, Puggina A, et al. Socio-economic determinants of physical activity across the life course: A “DEterminants of DIet and Physical ACtivity” (DEDIPAC) umbrella literature review. PLoS One. 2018;13(1):e0190737. doi:10.1371/journal.pone.0190737
31. Fulton M, Dadana S, Srinivasan VN. Obesity, Stigma, and Discrimination. In: StatPearls [Internet]. StatPearls Publishing; 2023. Accessed March 12, 2025. https://www.ncbi.nlm.nih.gov/books/NBK554571/
32. Rubino F, Puhl RM, Cummings DE, et al. Joint international consensus statement for ending stigma of obesity. Nature Medicine. 2020;26(4):485. doi:10.1038/s41591-020-0803-x
33. A meta-analysis of empirical studies of weight-based bias in the workplace. Journal of Vocational Behavior. 2009;74(1):1-10. doi:10.1016/j.jvb.2008.09.008
34. Puhl RM, Lessard LM, Himmelstein MS, Foster GD. The roles of experienced and internalized weight stigma in healthcare experiences: Perspectives of adults engaged in weight management across six countries. PLoS ONE. 2021;16(6):e0251566. doi:10.1371/journal.pone.0251566
35. Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obesity Reviews. 2015;16(4):319. doi:10.1111/obr.12266
36. Puhl RM, King KM. Weight discrimination and bullying. Best practice & research Clinical endocrinology & metabolism. 2013;27(2). doi:10.1016/j.beem.2012.12.002
37. Puhl R, Brownell KD. Bias, discrimination, and obesity. Obesity research. 2001;9(12). doi:10.1038/oby.2001.108
38. van Geel M, Vedder P, Tanilon J. Are overweight and obese youths more often bullied by their peers? A meta-analysis on the correlation between weight status and bullying. International journal of obesity (2005). 2014;38(10). doi:10.1038/ijo.2014.117
39. Rankin J, Matthews L, Cobley S, et al. Psychological consequences of childhood obesity: psychiatric comorbidity and prevention. Adolescent Health, Medicine and Therapeutics. 2016;7:125. doi:10.2147/AHMT.S101631
40. Chandrabose M, Rachele JN, Gunn L, et al. Built environment and cardio-metabolic health: systematic review and meta-analysis of longitudinal studies. Obes Rev. 2019;20(1):41-54. doi:10.1111/obr.12759
41. Yeager R, Riggs DW, DeJarnett N, et al. Association between residential greenness and cardiovascular disease risk. J Am Heart Assoc. 2018;7(24):e009117. doi:10.1161/JAHA.118.009117
42. Keith RJ, Hart JL, Bhatnagar A. Greenspaces and cardiovascular health. Circ Res. 2024;134(9):1179-1196. doi:10.1161/CIRCRESAHA.124.323583
43. Jaacks LM, Di Cesare M. The epidemiology and social determinants of obesity. Clinical Obesity in Adults and Children. Published online March 11, 2022:17-30. doi:10.1002/9781119695257.ch2
44. Rees-Punia E, Hathaway ED, Gay JL. Crime, perceived safety, and physical activity: A meta-analysis. Prev Med. 2018;111:307-313. doi:10.1016/j.ypmed.2017.11.017
45. Church TS, Thomas DM, Tudor-Locke C, et al. Trends over 5 Decades in U.S. Occupation-Related Physical Activity and Their Associations with Obesity. PLoS ONE. 2011;6(5):e19657. doi:10.1371/journal.pone.0019657
46. Solovieva S, Lallukka T, Virtanen M, Viikari-Juntura E. Psychosocial factors at work, long work hours, and obesity: a systematic review. Scandinavian journal of work, environment & health. 2013;39(3). doi:10.5271/sjweh.3364
47. Lavie CJ, Ozemek C, Carbone S, Katzmarzyk PT, Blair SN. Sedentary Behavior, Exercise, and Cardiovascular Health. Circulation research. 2019;124(5). doi:10.1161/CIRCRESAHA.118.312669
48. Tigbe WW, Granat MH, Sattar N, Lean MEJ. Time spent in sedentary posture is associated with waist circumference and cardiovascular risk. International journal of obesity (2005). 2017;41(5). doi:10.1038/ijo.2017.30
49. Kumar R, Rizvi MR, Saraswat S. Obesity and Stress: A Contingent Paralysis. International Journal of Preventive Medicine. 2022;13:95. doi:10.4103/ijpvm.IJPVM_427_20
50. Fardet L, Fève B. Systemic glucocorticoid therapy: a review of its metabolic and cardiovascular adverse events. Drugs. 2014;74(15). doi:10.1007/s40265-014-0282-9
51. McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: Links to socioeconomic status, health, and disease. Annals of the New York Academy of Sciences. 2010;1186:190. doi:10.1111/j.1749-6632.2009.05331.x
52. Steptoe A, Feldman PJ, Kunz S, Owen N, Willemsen G, Marmot M. Stress responsivity and socioeconomic status: a mechanism for increased cardiovascular disease risk? European heart journal. 2002;23(22). doi:10.1053/euhj.2001.3233
53. Subramanian S, Deaton A. The Demand for Food and Calories. Journal of Political Economy. 1996;104(1):133-162. Accessed March 28, 2025. https://EconPapers.repec.org/RePEc:ucp:jpolec:v:104:y:1996:i:1:p:133-62
54. Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2012;13(8). doi:10.1111/j.1467-789X.2011.00982.x
55. Urbanization without Growth : A Not-So-Uncommon Phenomenon. Published online August 2000. doi:10.1596/1813-9450-2412
56. Tschirley D, Reardon T, Dolislager M, Snyder J. The Rise of a Middle Class in East and Southern Africa: Implications for Food System Transformation. Journal of International Development. 2015;27(5):628-646. Accessed March 28, 2025. https://EconPapers.repec.org/RePEc:wly:jintdv:v:27:y:2015:i:5:p:628-646
57. Holdsworth M, Gartner A, Landais E, Maire B, Delpeuch F. Perceptions of healthy and desirable body size in urban Senegalese women. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 2004;28(12). doi:10.1038/sj.ijo.0802739
58. Lenardson JD, Hansen AY, Hartley D. Rural and Remote Food Environments and Obesity. Current obesity reports. 2015;4(1). doi:10.1007/s13679-014-0136-5
59. Liese AD, Weis KE, Pluto D, Smith E, Lawson A. Food store types, availability, and cost of foods in a rural environment. Journal of the American Dietetic Association. 2007;107(11). doi:10.1016/j.jada.2007.08.012
60. Seguin R, Connor L, Nelson M, LaCroix A, Eldridge G. Understanding barriers and facilitators to healthy eating and active living in rural communities. Journal of nutrition and metabolism. 2014;2014. doi:10.1155/2014/146502
61. Gilmore AB, Fabbri A, Baum F, et al. Defining and conceptualising the commercial determinants of health. Lancet. 2023;401(10383):1194-1213. doi:10.1016/S0140-6736(23)00013-2
62. Commercial determinants of NCDs. Accessed March 12, 2025. https://www.who.int/europe/teams/special-initiative-on-ncds-and-innovation/commercial-determinants-of-ncds
63. Trang K, Grant SFA. Genetics and epigenetics in the obesity phenotyping scenario. Rev Endocr Metab Disord. 2023;24(5):775-793. doi:10.1007/s11154-023-09804-6
64. Liu BN, Liu XT, Liang ZH, Wang JH. Gut microbiota in obesity. World J Gastroenterol. 2021;27(25):3837-3850. doi:10.3748/wjg.v27.i25.3837
65. Morton GJ, Cummings DE, Baskin DG, Barsh GS, Schwartz MW. Central nervous system control of food intake and body weight. Nature. 2006;443(7109). doi:10.1038/nature05026
66. Hall KD, Heymsfield SB, Kemnitz JW, Klein S, Schoeller DA, Speakman JR. Energy balance and its components: implications for body weight regulation. The American journal of clinical nutrition. 2012;95(4). doi:10.3945/ajcn.112.036350
67. Pontzer H, Raichlen DA, Wood BM, Mabulla AZP, Racette SB, Marlowe FW. Hunter-Gatherer Energetics and Human Obesity. PLoS ONE. 2012;7(7):e40503. doi:10.1371/journal.pone.0040503
68. Bray GA, Kim KK, Wilding JPH. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2017;18(7). doi:10.1111/obr.12551
69. Okunogbe A, Nugent R, Spencer G, Powis J, Ralston J, Wilding J. Economic impacts of overweight and obesity: current and future estimates for 161 countries. BMJ Glob Health. 2022;7(9). doi:10.1136/bmjgh-2022-009773
70. Gannon J, Pollock AJ, Allen DB, Kling PJ. A Practical Screening Tool to Predict Early Childhood Obesity Risk: Examining a Birth Cohort. Clinical pediatrics. 2020;60(3):178. doi:10.1177/0009922820971006
71. Ryan DH, Deanfield JE, Jacob S. Prioritizing obesity treatment: expanding the role of cardiologists to improve cardiovascular health and outcomes. Cardiovasc Endocrinol Metab. 2023;12(1):e0279. doi:10.1097/XCE.0000000000000279
72. Flint SW. Rethinking the label anti-obesity medication. Lancet Diabetes Endocrinol. 2024;12(5):301-302. doi:10.1016/S2213-8587(24)00071-8
73. Lincoff AM, Brown-Frandsen K, Colhoun HM, et al. Semaglutide and cardiovascular outcomes in obesity without diabetes. N Engl J Med. 2023;389(24):2221-2232. doi:10.1056/NEJMoa2307563
74. Kosiborod MN, Abildstrøm SZ, Borlaug BA, et al. Semaglutide in patients with heart failure with preserved ejection fraction and obesity. N Engl J Med. 2023;389(12):1069-1084. doi:10.1056/NEJMoa2306963
75. Packer M, Zile MR, Kramer CM, et al. Tirzepatide for heart failure with preserved ejection fraction and obesity. N Engl J Med. 2025;392(5):427-437. doi:10.1056/NEJMoa2410027
76. Badve SV, Bilal A, Lee MMY, et al. Effects of GLP-1 receptor agonists on kidney and cardiovascular disease outcomes: a meta-analysis of randomised controlled trials. The lancet Diabetes & endocrinology. 2025;13(1). doi:10.1016/S2213-8587(24)00271-7
77. Bianchettin RG, Lavie CJ, Lopez-Jimenez F. Challenges in cardiovascular evaluation and management of obese patients: JACC state-of-the-art review. J Am Coll Cardiol. 2023;81(5):490-504. doi:10.1016/j.jacc.2022.11.031
78. Koskinas KC, Van Craenenbroeck EM, Antoniades C, et al. Obesity and cardiovascular disease: an ESC clinical consensus statement. Eur J Prev Cardiol. 2025;32(3):184-220. doi:10.1093/eurjpc/zwae279
79. World Health Organization. Compendium of WHO and Other UN Guidance on Health and Environment: Version with International Classification of Health Intervention (ICHI) Codes. World Health Organization; 2024. https://play.google.com/store/books/details?id=xaMOEQAAQBAJ
80. World Health Organization. Health Service Delivery Framework for Prevention and Management of Obesity. World Health Organization; 2023. https://play.google.com/store/books/details?id=26IOEQAAQBAJ
81. Nieuwenhuijsen MJ. Influence of urban and transport planning and the city environment on cardiovascular disease. Nat Rev Cardiol. 2018;15(7):432-438. doi:10.1038/s41569-018-0003-2
82. World Health Organization. Healthy Cities Effective Approach to a Rapidly Changing World. World Health Organization; 2020. https://play.google.com/store/books/details?id=4nYOEQAAQBAJ
83. World Health Organization-Regional Office for Europe. Healthy Cities tackle the social determinants of inequities in health: A framework for action. 2012. Accessed March 11, 2025. http://www.euro.who.int/pubrequest
84. World Health Organization. Fiscal Policies for Diet and Prevention of Noncommunicable Diseases - Technical Meeting Report, 5-6 May 2015. 2015. Accessed March 11, 2025. https://www.who.int/docs/default-source/obesity/fiscal-policies-for-diet-and-the-prevention-of-noncommunicable-diseases-0.pdf?sfvrsn=84ee20c_2
85. World Health Organisation. Global action plan for the prevention and control of noncommunicable diseases 2013-2020. 2013. Accessed March 11, 2025. https://www.who.int/publications/i/item/9789241506236
86. National Research Council (US). The Public Health Effects of Food Deserts: Workshop Summary. National Academies Press (US); 2009. doi:10.17226/12623
87. World Health Organization. School policy framework : implementation of the WHO global strategy on diet, physical activity and health. 2008. Accessed March 11, 2025. https://apps.who.int/iris/bitstream/handle/10665/43923/9789241596862_eng.pdf
88. World Health Organization. Global Strategy on Diet, Physical Activity and Health. 2002. Accessed March 11, 2025. https://iris.who.int/bitstream/handle/10665/43035/9241592222_eng.pdf?sequence=1
89. den Braver NR, Garcia Bengoechea E, Messing S, et al. The impact of mass-media campaigns on physical activity: a review of reviews through a policy lens. Eur J Public Health. 2022;32(Suppl 4):iv71-iv83. doi:10.1093/eurpub/ckac085
90. Pallan M, Adab P. Preventing obesity through school based approaches to improve nutrition. BMJ Med. 2023;2(1):e000463. doi:10.1136/bmjmed-2022-000463
91. Toolkit for Developing a Multisectoral Action Plan for Noncommunicable Diseases. Module 5. Evaluating the Implementation of a Multisectoral Action Plan. World Health Organization; 2022. https://play.google.com/store/books/details?id=RXRyEAAAQBAJ
92. Publications. World Obesity Federation Global Obesity Observatory. Accessed March 28, 2025. https://data.worldobesity.org/publications/wof-health-systems-final
93. PARIS. A new cycling plan for a 100% bikeable city. 2024. Accessed March 11, 2025. https://www.paris.fr/en/pages/a-new-cycling-plan-for-a-100-bikeable-city-28350#:~:text=The%202021%2D2026%20cycling%20
plan,and%20an%20enhanced%20cycling%20ecosystem
94. Brown H, Xiang H, Albani V, et al. No new fast-food outlets allowed! Evaluating the effect of planning policy on the local food environment in the North East of England. Soc Sci Med. 2022;306(115126):115126. doi:10.1016/j.socscimed.2022.115126
95. DOF - Diario Oficial de la Federación. Accessed March 11, 2025. https://www.dof.gob.mx/nota_detalle.php?codigo=5325371&fecha=11/12/2013#gsc.tab=0
96. Global Health Advocacy Incubator. Brazil implements front-of-package warning labels. 2022. Accessed March 11, 2025. https://www.advocacyincubator.org/news/2022-11-08-brazil-implements-front-of-package-warning-labels#:~:text=These%20efforts%20culminated%20with%20the,sugar%2C%20saturated%20fats%20and%20sodium
97. U.S. Department of Agriculture-Rural Development. Healthy Food Financing Initiative. Accessed March 11, 2025. https://www.rd.usda.gov/about-rd/initiatives/healthy-food-financing-initiative#:~:text=The%20HFFI%20Programme%20provides%20funding,through%20SNAP%20eligible%20food%20retailers
98. Finnish National Agency for Education. School Meals in Finland. Accessed March 11, 2025. https://www.oph.fi/en/education-and-qualifications/school-meals-finland
99. Food Safety and Standards Authority of India. Eat Right India. Accessed March 11, 2025. https://eatrightindia.gov.in/eatrightindia.jsp
100. Miyoshi M, Tsuboyama-Kasaoka N, Nishi N. School-based “Shokuiku” programme in Japan: application to nutrition education in Asian countries. Asia Pac J Clin Nutr. 2012;21(1):159-162. https://pubmed.ncbi.nlm.nih.gov/22374574/
101. Benefits C. Cisco Purpose Reporting Hub. Accessed March 11, 2025. https://www.cisco.com/c/m/en_us/about/csr/esg-hub/people/benefits.html
102. PROGRAMMEME NATIONAL NUTRITION SANTÉ. Accessed March 11, 2025. https://sante.gouv.fr/IMG/pdf/pnns4_2019-2023.pdf
103. EUR-Lex - 52020DC0381 - EN - EUR-Lex. Accessed March 11, 2025. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:52020DC0381
104. Nipers A, Upite I, Pilvere I, Stalgiene A, Viira AH. Effect of VAT rate reduction for fruits and vegetables on prices in Latvia: ex-post analysis. Published online 2019. doi:10.15159/JAS.19.06
105. Lives H. Mana Tū - Healthier Lives. Accessed March 11, 2025. https://healthierlives.co.nz/research/mana-tu/
106. Rwanda Social Security Board. CBHI Scheme. Accessed March 11, 2025. https://www.rssb.rw/scheme/cbhi-scheme
107. UNICEF, City of Amsterdam, EAT, TheAmsterdam Healthy Weight Approach: Investing inhealthy urban childhoods: A case study on healthydiets for children, 2020